Blog
Teeth whitening
Teeth whitening can be safe when done under the guidance of a dental professional or by following the instructions of over-the-counter products. However, it’s important to be aware of potential side effects, such as tooth sensitivity or gum irritation. Consult your dentist to discuss the best and safest whitening options for your specific needs.
Methods of teeth whitening:
**Professional Whitening:**This is done by a dentist and is the most effective method. It can involve in-office treatments using strong bleaching agents or custom-fitted trays with professional-grade whitening gels.
**Over-the-Counter (OTC) Products:** These include whitening toothpaste, strips, and gels. They are less potent than professional treatments and may take longer to show results.
Benefits of teeth whitening:
Improved Aesthetics: Whitening can remove stains and discoloration, enhancing the appearance of your teeth.
Boosted Confidence: A brighter smile often leads to increased self-confidence.
Non-Invasive: It’s a non-surgical and minimally invasive cosmetic dental procedure.
Risks and considerations:
Tooth Sensitivity: Whitening can cause temporary sensitivity to hot or cold foods and beverages.
Gum Irritation: Overuse or improper application of whitening products can irritate the gums.
Uneven Results: Whitening may not be equally effective on all teeth, leading to uneven results.
Duration of Effect: The duration of whitening effects varies; it may require touch-ups to maintain results.
Pre-existing Dental Issues: Whitening may not be suitable for everyone, especially those with dental restorations (crowns, fillings) as they do not respond to whitening treatments.
It’s crucial to consult with a dentist to discuss your specific needs and any potential risks associated with teeth whitening. They can help you choose the most appropriate and safe method for your situation.
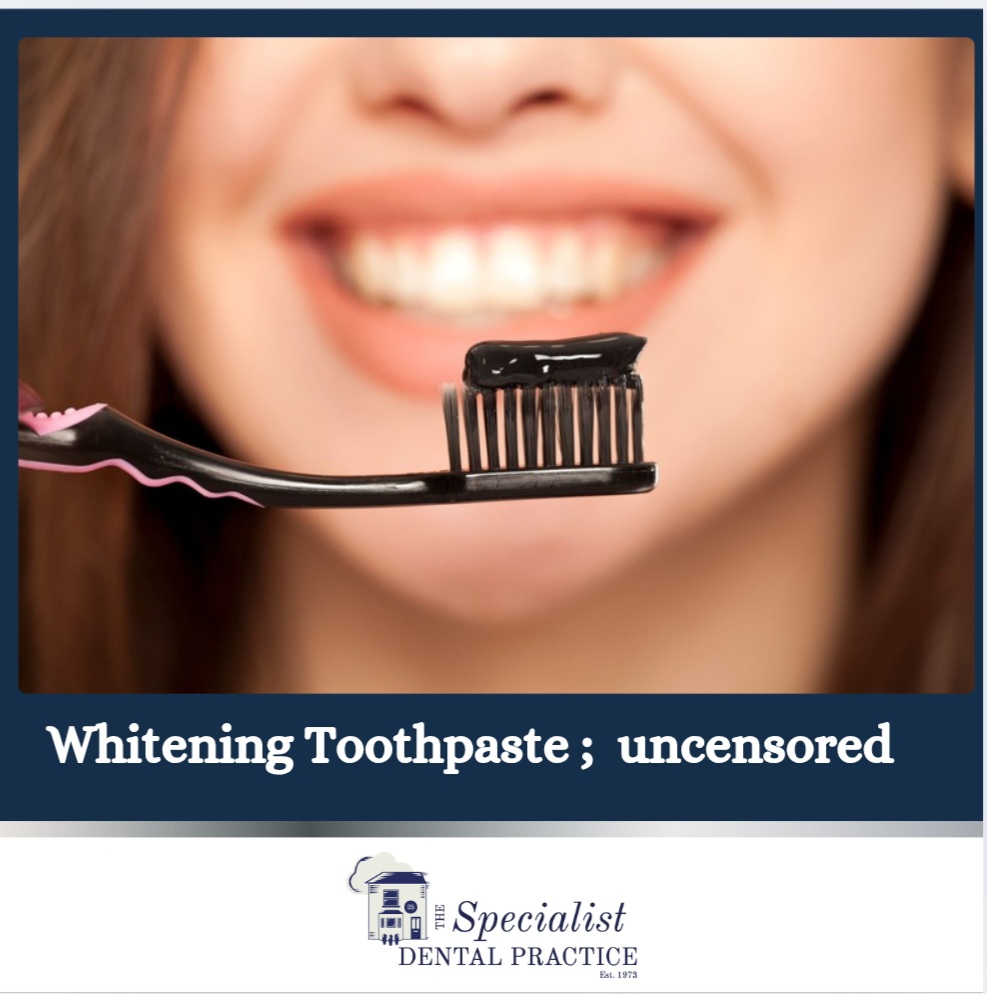
Whitening Toothpastes; Facts and Fallacies
A Guide to Whitening Toothpastes in the UK: Efficacy Backed by Clinical Evidence
Whitening toothpastes are a popular choice for enhancing smiles, but how effective are they? In this blog, we’ll explore different types of whitening toothpastes available in the UK and evaluate their efficacy based on clinical evidence.
Abrasive-Based Whitening Toothpastes
These use mild abrasives like silica to remove surface stains caused by food, drinks, or smoking. While they can visibly improve brightness, clinical studies show they only remove extrinsic stains without altering the tooth’s natural color.
Efficacy: Effective for surface stain removal but not for deeper discoloration.
Enzyme-Based Whitening Toothpastes
Enzyme-based formulations (e.g., containing papain or bromelain) target protein pellicles that cause staining. Evidence suggests they can enhance stain removal without excessive abrasion, making them suitable for sensitive teeth.
Efficacy: Moderate improvement in surface brightness with minimal damage to enamel.
Peroxide-Based Whitening Toothpastes
Some toothpastes contain low levels of hydrogen or carbamide peroxide. Studies indicate they can help lighten intrinsic stains with consistent use over weeks. However, their whitening effect is less significant compared to professional bleaching.
Efficacy: Proven for mild intrinsic whitening, though results are subtle.
Charcoal Whitening Toothpastes
Charcoal-based products are widely marketed for whitening, but clinical evidence shows limited efficacy in removing stains. Excessive use may even harm enamel and gums due to high abrasiveness.
Efficacy: Poor stain removal with potential enamel damage.
Blue Covarine-Infused Toothpastes
These provide an immediate optical effect by depositing a blue pigment on teeth, creating the illusion of whiteness. While the results are temporary, studies support their effectiveness for a quick enhancement.
Efficacy: Temporary improvement in tooth brightness, ideal for short-term use.
Key Takeaways
Best for Surface Stains: Abrasive or enzyme-based toothpastes.
For Intrinsic Whitening: Peroxide-based formulas are most effective but offer mild results.
Quick Fix: Blue covarine toothpastes.
Avoid Overuse: Charcoal toothpastes due to abrasiveness.
For significant whitening or intrinsic stains, professional treatments remain the gold standard. Always consult your dentist to ensure the safest and most effective solution for your smile.
Dental Care and Coronavirus (COVID-19)
It is likely that the coronavirus will have an effect on your dental care.
Routine dental check-ups have been cancelled, and ongoing treatment plans may be disrupted. Where and how you access emergency dental treatment could also change.
This page includes advice on how you can access dental care, treatment and advice during the coronavirus pandemic.
Visiting the dental practice
If you are suffering with your oral health and need support, we are here to help.
To help stop the spread of coronavirus, we are advising against all routine and non-urgent dental treatment.
This includes:
Dental check-ups.
Preventive treatments such as scale and polish and fluoride varnishes.
Examinations and x-rays.
Appointments for braces.
Cosmetic dental treatment of any kind e.g. tooth whitening.
Routine denture treatment.
Treatments on teeth that are not painful e.g. fillings and extractions.
It is likely that your dental practice will contact you to postpone these appointments. If you do not hear from your dental practice, we recommend that you contact them to cancel your appointment and rearrange it for a later date.
In accordance to the instructions received by Public Health England (PHE) and CQC, all dental practices in England have temporarily ceased routine and non-urgent dental treatment. For emergency and urgent dental treatment, the dental surgery will provide remote (telephone or video-link) advice and assessment for further referral to the dedicated NHS Urgent Dental Care Centres (UDC) if necessary.
Whenever possible, stay at home and help stop the spread of coronavirus. This includes people of all ages – even if you do not have any symptoms or other health conditions.
Non-necessary dental treatment is not a reason for you to leave the home.
Urgent Dental Care
The NHS England has set up dedicated Urgent Dental Care Centres (UDC) for emergency and urgent dental conditions. Please note that this is not a walk-in service and requires appropriate referral by your dentist following remote triage.
If you are in pain, bleeding, swelling, or have had an accident and need urgent dental care, please contact your dental practice.
Please do not visit your dental practice without calling them first.
If you are not registered with any dental practice, please call 111 for further advice.
Dental Treatments in hospitals and A&E
To support NHS services and protect vital resources, it is important that you do not visit hospitals or A&E departments with dental problems.
If you need urgent or emergency dental treatment, contact your dental practice and they will be able to triage and direct you.
Dental care for vulnerable people and those with symptoms
If you need urgent dental care and are self-isolating because you have symptoms relating to coronavirus, or are a vulnerable person at higher risk, call NHS 111 or your dental practice.
The dental practice will be able to assess your needs and if necessary refer you to a special team/centre who will be able to treat you.
Buying oral health products
There is no shortage of oral health products like toothbrushes, toothpaste and mouthwash. Because of this, there is no need to stockpile them.
It is important to only buy what you need, when you need it.
Supermarkets remain open for essential food shopping and we advise that you buy any oral health products you need during this time. Please remember however to keep to social distancing rules and maintain two metres away from other shoppers.
When possible, instead of visiting supermarkets, we recommend that you buy oral health products online and have them delivered to your home.
Tips for good oral health
To help prevent dental problems from happening during coronavirus, here are some top tips for good oral health.
- Brush your teeth for two minutes, twice a day with a fluoride toothpaste.
- Do not share your toothbrushes. Keep the toothbrush clean and replace them frequently.
- The best time to brush is first thing in the morning and last thing at night before you go to bed.
- Cut down on how much sugar you have and how often you have it. This is even more important for children at home with increased temptation to snack and consume high sugar diet.
- Keep sugar consumption to mealtimes. This will reduce the time your teeth are under acid -attack.
- Maintain good hydration and avoid smoking and excessive consumption of alcohol.
- Use interdental brushes or floss to clean in between the teeth.
- Use non-alcohol based mouthwash daily to remove bad bacteria and keep fresh breath.
- Sugar-free chewing gum can help produce saliva and neutralise the plaque acids in your mouth.
More information and advice
Children coronavirus fact sheet, click here
For information about the coronavirus (COVID-19), please visit www.nhs.uk/conditions/coronavirus-covid-19/
The desire for the perfect Hollywood smile but at what cost?!

Cosmetic dentistry has become increasingly popular, largely as a result of social trends and increased media coverage. With the reality TV stars setting the trend in an industry now worth £2 billion, this understandable desire for the alleged ‘perfect smile’ needs to be tempered with an appropriate awareness of the significant risks associated with invasive cosmetic procedures such as veneers and crowns.
Patients need to be properly informed that elective removal of healthy enamel and dentine can result in pulpal injury and poorer periodontal health in the longer term, particularly if they are young. The duty of candour means that they ought to be informed that aggressive reduction of sound tooth tissue is not biologically neutral and results in structural weakening of their teeth. Less invasive procedures such as bleaching on its own or for example, combined with direct resin composite bonding, can satisfy many patient’s demands, while still being kinder to teeth and having much better fall-back positions for their future requirements.
It is the opinion of the British Endodontic Society, British Society for Restorative Dentistry, Restorative Dentistry UK, Dental Trauma UK, British Society of Prosthodontics and the British Society of Paediatric Dentistry that elective invasive cosmetic dental treatments can result in great benefit to patients, but that some aggressive treatments used to achieve them can produce significant morbidities in teeth which were previously healthy. This is a worrying and growing problem with many ethical, legal and biologic aspects, but many adverse outcomes for patients who request cosmetic dental improvements are preventable by using biologically safer initial approaches to treatment planning and its provision.
Dedicated personal, specialist care
The Specialist Dental Practice is the leading specialist restorative and implant dental practice in the county and has been setting the standards of specialist dentistry over the last 25 years.
The practice was established in 1973 and is conveniently located in the heart of Weybridge, Surrey. We are UK qualified and registered multi-specialist team offering specialist dental care of the highest quality and precision for the complex reconstruction cases involving dental implant therapy, gum disease treatment, root canal treatment, restoration of mutilated dentition and addressing challenges associated with partial and complete removable dentures.
We are delighted to welcome new referrals to our practice from both patients as well as professional colleagues.
Dental Implants
Essential questions to ask your dentist on dental implants
Taking the decision to have dental implants treatment is something most people will wish to consider quite carefully. Although this treatment can be an excellent long-term solution, it isn’t right for everybody and it is important to have a good understanding of exactly what is required. We have outlined a few essential questions and points you should be aware of before making your final decision.
WHAT ARE YOUR QUALIFICATIONS AND EXPERIENCE IN PLACING DENTAL IMPLANTS?
This is the most important question to ask and should be top of your list. Some clinicians have minimal training in placing dental implants and may only carry out this type of surgery a few times a year.
Our specialist care is based on dental specialties that are officially recognised by the General Dental Council UK. All accredited dental specialists are listed on the General Dental Council website www.gdc-uk.org. The specialist lists exist to:
• ensure high standards of training and assessment qualifying dentists to use a specialist title;
• indicate those dentists who possess recognised specialist knowledge, skills and attitudes;
• protect patients against unwarranted claims to be a specialist;
• facilitate appropriate referrals of patients;
• promote high standards of care by dentists qualified to use a specialist title; and
• encourage postgraduate education.
This list helps patients make an informed decision when they are looking for appropriately trained dentists to manage their dental care.
WHICH IMPLANT SYSTEMS DO YOU USE?
There are a few major dental implant companies that produce high-quality dental implants backed by years of research. These companies are well-known and well respected within the dental industry. There are numerous other companies that produce generic dental implants.
While these may still be of an acceptable quality, they lack the provenance of more widely known dental implant systems. There is another benefit of choosing dental implants made by one of the major companies as these implants are used worldwide. When you need an implant repaired or a component replaced or maintained, it is much easier to find a dentist willing to do this for you, no matter where you are in the world.
DO YOU PROVIDE COMPUTER GUIDED DENTAL IMPLANTS?
Computer guided dental implants surgery involves precisely planning using advanced diagnostics that include a cone beam CT scan and planning software. Once everything is planned, this computerised information is used to create a surgical guide or stent which allows precise placement of each implant.
We prefer to execute guided surgery where possible as it ensures your implant surgery is smoother, quicker and ultimately more comfortable and successful. Not all dentists will use this technique, but it is especially important when placing multiple implants where precision placement is even more vital.
Research shows that appropriately and precisely placed dental implants are less likely to have any problems and complications.
WILL IMPLANT SURGERY HURT?
You should not feel any pain during surgery based on effective local anaesthesia. We know many patients feel anxious at the thought of any oral surgery and if this applies to you then we can discuss additional sedation.
Our dental team is also very experienced at helping nervous patients feel at ease. Most of our patients will report no or very minimal discomfort that is very well managed with simple painkillers following implant surgery.
WILL I NEED A LONG TIME TO RECOVER AFTER IMPLANT SURGERY?
If you need just a single dental implant, you should be back to work the very next day. If you have multiple dental implants you might need a bit longer to recover; your dental implant dentist can give you more advice based on your situation.
Although you may feel some minor discomfort once the anaesthesia wears off, it is not uncommon to feel perfectly fine, especially after single dental implant placements. Again, this is something that can be discussed during your first consultation as it will depend on your treatment.
HOW LONG WILL IT TAKE TO COMPLETE IMPLANT TREATMENT?
Dental implant treatment can take up to several months to complete, as the surgery must be planned and once in place the implants need time to heal. It generally takes about 8-12 weeks for the dental implants to fully heal and to integrate with your jawbone, and the crown or bridge can be placed shortly after. Treatment may take slightly longer if you need bone grafts or tissue regeneration.
WILL I BE LEFT WITHOUT TEETH DURING IMPLANT HEALING?
This is a major concern for many people but there is no need to worry as temporary teeth can be provided while your implants heal. These temporary restorations can be fabricated before your implant surgery and may be placed immediately after surgery is completed.
WILL MY NEW IMPLANT TEETH LOOK NATURAL?
It is essential that your dental implants are placed in precisely the right position for the best functional and aesthetic effects. Here, at The Specialist dental Practice, our team are specialists in restoring and replacing missing teeth with crowns, bridges and dentures to the highest standards ensuring your new teeth are designed to look and feel wonderful. We also offer aftercare and advice on how to keep your implants clean.
HOW CAN I STOP MY DENTAL IMPLANTS FROM FAILING?
While some implants will fail naturally, a large part of implant success comes down to two factors:
• How well the implant is placed and the correct positioning in the jaw
• How well the implant is cared for after placement
Choosing a qualified and skilled implant dentist who is able to plan the correct positioning for your dental implants is key. Whilst you may think a general dentist is slightly cheaper, you may end up paying more in the future with implants that have not been placed correctly with significant potential complications.
The biggest misconception from dental implant patients is that once your dental implants are placed they will be there for life and are indestructible. The fact is, you will need to take care of your dental implants and make sure you regularly attend check-ups and clean your implants properly. Without this, your implants will have a larger chance of failing, both in a biologic and hardware sense.
SHOULD I GO ABROAD TO HAVE DENTAL IMPLANTS?
Dental tourism’ is a concept that has become increasingly popular over the last decade. Patients seek out dental treatment such as dental implants abroad and travel for the sole purpose of receiving cosmetic and restorative dentistry. The main attraction for patients is the cost of treatment in some other countries – it can look like prices are significantly cheaper, depending on the individual treatments. However, as with many things in life, what looks too good to be true often is. There are all kinds of hidden costs with choosing to get dental implants abroad including the prohibitive costs to fix a failing dental implant placed abroad, variation in the standard of care, and lack of long- term aftercare and maintenance plan.
Should you wish to seek more information on dental implant therapy, please contact the practice on 01932857585 or get in touch online info@weybridgedentist.co.uk to arrange for a consultation. In that way, we can assess for your individual needs and provide you with a customised treatment plan .
Specialist treatment for gum disease affecting teeth and dental implants

Understanding the importance of gum health
Gum disease affects many aspects of our life but is often overlooked as it has few symptoms in its early stages – that’s why it is often called ‘the silent disease’.
The vital thing about gum disease is that it is highly preventable and, especially in the early stages, quite easily treatable. Many studies link oral health to a number of significant conditions. There is strong evidence of the links between diabetes and gum disease. For Alzheimer’s and cardio health the role of gum disease is less clear. More than 45% of adults in the UK are affected by gum disease and, even at its most mild level, it can affect your quality of life.
Gum disease can affect dental implants as much as natural teeth. If you have any concerns about your dentition, speak to us and we will be happy to work with your dentist in managing your case.
Saving Your Natural Tooth
Specialist Endodontic Treatment
Nothing looks, feels or functions like your natural teeth, and endodontists are the experts in saving teeth. Keep smiling and eating the foods you love with endodontic treatment that can relieve your pain and save your teeth.
Sometimes your teeth may have infection or disease and will need additional care. When possible, you should always consider treatments to save your teeth. You may think, why not have a tooth pulled, especially if no one can see it, but you will know your tooth is missing and it will negatively impact your quality of life.
Don’t get a tooth pulled because you think its easier or more cost-effective. Missing teeth can cause other teeth to shift, affect your ability to properly chew and ruin your smile. Tooth extraction often is more painful than the infection itself, and replacing an extracted tooth with an artificial one requires additional dental visits that can quickly add up.
Modern endodontics offers advancements in technologies, procedures and materials, giving you many treatment options to save your natural teeth. It’s important to understand your choices and how they’ll impact both your tooth and your future dental health. It’s always best to retain your natural teeth whenever possible and endodontic treatment should be your first choice for the best health and cosmetic results. Endodontists are specialists in saving teeth. They can evaluate your condition and provide the best treatment plan to help you save your teeth for a lifetime.
Here are some tips for saving your teeth:
- When given a choice between tooth extraction and root canal treatment, always opt for a root canal. No denture, bridge or implant will look, feel and function as well as a natural tooth.
- Act immediately when you experience symptoms of swelling or pain. Most endodontists can accommodate emergency cases, even on weekends, ensuring you’ll be seen quickly.
- If your dentist recommends tooth extraction, ask whether the root canal is an option.If you’re told root canal is not an option, ask why and request a referral to an endodontist.
Root canal treatment from an endodontist is virtually painless and often leaves you with less discomfort during recovery than if you have your natural tooth extracted. Thanks to modern techniques and effective anesthesia, patients who experience root canals are six times more likely to describe it as painless than patients who have a tooth extracted! Take the time to learn more about root canal treatment and some of the common misconceptions about it and then take the first step to a pain-free, healthy mouth by visiting an endodontist.
How does endodontic treatment save the tooth?
It’s necessary to have endodontic or root canal treatment when the inside of your tooth (the pulp) becomes inflamed or infected as a result of deep decay, repeated dental procedures, faulty crowns or a crack or chip in the tooth. Trauma to your tooth may also cause pulp damage even if the tooth has no visible chips or cracks. If pulp inflammation or infection is left untreated, it can cause pain or lead to an abscess.
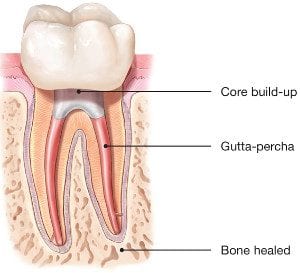
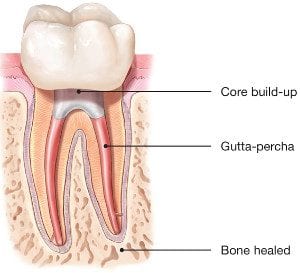
When you undergo a root canal or other endodontic treatment, the inflamed or infected pulp is removed and the inside of the tooth is carefully cleaned and disinfected, then filled and sealed with a rubber-like material called gutta-percha. Afterward, the tooth is restored with a crown or filling for protection and will continue to function like any other tooth.
Endodontic treatment helps you maintain your natural smile, continue eating the foods you love and limits the need for ongoing dental work. With proper care, most teeth that have had root canal treatment can last a lifetime.
For more detailed information on root canal or to organise for a consultation, call us or get in touch online.
Biomimetic Dentistry
What is Biomimetic Dentistry?

Translated literally, biomimetic dentistry means to copy what is life-like. Nature has provided the most successful and ideal properties to our natural teeth. When restoring damaged, broken, and decayed teeth, the goal is to return the tooth to its original strength, function, and esthetics. Biomimetic dentistry accomplishes all of this in a conservative, strong, and attractive approach.
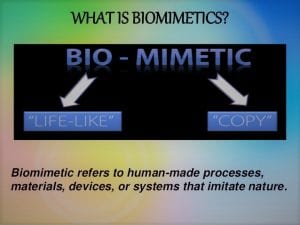
Why is it so important?
Tooth preservation and dental conservation lie at the heart of biomimetic dentistry.
Biomimetic dentistry replicates the strength, function, and aesthetics of natural teeth by replacing only damaged, decayed, and broken tooth structure. The principle employs techniques and materials that provide a perfect balance of nature, art and science.
Teeth move, bend and have physical dynamics of force that must be accounted for while re-making the tooth with nature as our guide. Much of the amputation of tooth structure can be eliminated with modern science. We can say that tooth preservation and dental conservation lie at the heart of biomimetic dentistry.
The economic implications of not needing the advanced, invasive care seen in traditional (amputational) dentistry have profound positive effects on people’s lives. We can now help patients create healthy and happy mouths with simple, and often painless techniques!
Patients are happier and often spend less compared to conventional treatment.
Give us a call to find out more or book a consultation appointment.
Want to stop snoring?
As a condition that affects over 40% of the population, it is no surprise that the majority of us have been impacted by snoring in some way, shape or form. There are both varying degrees and varying types of snoring: it can be ‘simple’, or it can be symptomatic and may require further exploration. Regardless, there are a number of conditions associated, including:
- diminished energy
- lack of concentration
- increased risk of stress
- reduced libido
- high blood pressure
As well as the impact to the snorer, a lack of sleep on the bed partner’s behalf is also dangerous for their health and well-being. Many cases are reported by the bed-partner, with the snorer having very little awareness of their bedtime activities.

Thankfully, there are many interventions that can assist with snoring. Before discussing these, however, it is first important to highlight the cause.
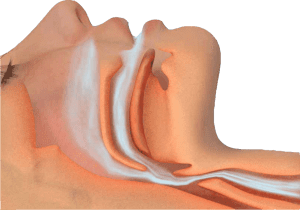
What causes snoring?
Once we are asleep, our muscles relax. This can result in the soft tissues in the throat vibrating, causing the familiar snoring sound.
However, this doesn’t happen to everyone: there are a number of factors that can increase chances of snoring, including: obesity, gender, age, alcohol, and medication. For most sufferers, snoring occurs in isolation (simple snoring). In these cases, it is often the bed-partner that suffers, with the snorer unaware that they are causing such a disturbance. However, it can also take place as part of a more serious condition, obstructive sleep apnoea, which can be potentially life-threatening if not treated correctly.
What is obstructive sleep apnoea (OSA)?
OSA is a serious condition where, for short periods of time, the airway becomes blocked during sleep, cutting off oxygen reaching the lungs. There are two types of breathing disruption associated with OSA:
- Apnoea – where the muscles collapse sufficiently enough to cause a total blockage of the airway for 10 seconds or more
- Hypopnoea – partial blockage of the airway that causes an airflow reduction of more than 50% for 10 seconds or more
Both of these problems can occur several times throughout the night and are most commonly recognised by loud snoring, paired with snorts, gasps, or laboured breathing. This leads to disruption for both the bed-partner AND the sufferer, with the snorer often waking feeling tired due to a night with reduced oxygen intake.
There are many associations with obstructive sleep apnoea, and, due to fat distribution, middle-aged males are twice as likely to suffer from OSA in comparison to middle-aged females. The discrepancy does start to level out, however, believed to be due to hormonal changes after menopause.
What are the treatments for snoring?
Though many snorers and tired bed-partners typically look to their doctor for help when it comes to snoring, their dentist arguably has a larger part to play – initially at least.
As snoring is typically caused by the lower jaw dropping back during sleep, the easiest way to stop it is to prevent the jaw from slipping backwards. This can be achieved with a device called a Mandibular Advancement Splint (MAS). Available from trained dentists, there are a number of devices available, one of which is the Sleepwell.

The most clinically proven MAS for the treatment of snoring & mild to moderate sleep apnoea, the Sleepwell is a two-piece device that is fully-adjustable by the wearer, and designed to hold your lower jaw forward. Holistically, however, there may be other behaviours that could assist with the problem, such as:
- Sleeping position – lying on your back inevitably is the worst position for snoring. Trying different positions may have a positive effect.
- Bed-time ‘hygiene’ – avoiding alcohol or caffeine in the evenings can help. Both muscle relaxants, they can increase the chances of snoring.
- Weight-loss – holding excess fat around your neck can play a major role in both snoring and sleep apnoea.
National Stop Snoring Week 23-27 April 2018
Cosmetic Dentistry- What You Should Know

Cosmetic dentistry has become increasingly popular, largely as a result of social trends and increased media coverage. This understandable desire for the alleged ‘perfect smile’ needs to be tempered with an appropriate awareness of the significant risks associated with invasive cosmetic procedures such as veneers and crowns. Patients need to be properly informed that elective removal of healthy enamel and dentine can result in pulpal injury and poorer periodontal health in the longer term, particularly if they are young. The duty of candour means that they ought to be informed that aggressive reduction of sound tooth tissue is not biologically neutral and results in structural weakening of their teeth. Less invasive procedures such as bleaching on its own or for example, combined with direct resin composite bonding, can satisfy many patient’s demands, while still being kinder to teeth and having much better fall-back positions for their future requirements. It is the opinion of the British Endodontic Society, British Society for Restorative Dentistry, Restorative Dentistry UK, Dental Trauma UK, British Society of Prosthodontics and the British Society of Paediatric Dentistry that elective invasive cosmetic dental treatments can result in great benefit to patients, but that some aggressive treatments used to achieve them can produce significant morbidities in teeth which were previously healthy. This is a worrying and growing problem with many ethical, legal and biologic aspects, but many adverse outcomes for patients who request cosmetic dental improvements are preventable by using biologically safer initial approaches to treatment planning and its provision.
Mouth Cancer Awareness Month

Most people have heard of cancer affecting parts of the body such as the lungs or breasts. However, cancer can also occur in the mouth, where the disease can affect the lips, tongue, cheeks and throat.
Anyone can be affected by mouth cancer, whether they have their own teeth or not. Mouth cancers are more common in people over 40, particularly men. However, research has shown that mouth cancer is becoming more common in younger patients and in women. In the last year more than 7,000 have been diagnosed with mouth cancer in the UK – an increase of more than a third compared to a decade ago.
Sadly, more than 1,800 people in the UK lose their life to mouth cancer every year. Many of these deaths could be prevented if the cancer was caught early enough. As it is, people with mouth cancer are more likely to die than those having cervical cancer or melanoma skin cancer.
Find out more at http://www.mouthcancer.org
Teeth whitening
Teeth whitening can be safe when done under the guidance of a dental professional or by following the instructions of over-the-counter products. However, it’s important to be aware of potential side effects, such as tooth sensitivity or gum irritation. Consult your dentist to discuss the best and safest whitening options for your specific needs.
Methods of teeth whitening:
**Professional Whitening:**This is done by a dentist and is the most effective method. It can involve in-office treatments using strong bleaching agents or custom-fitted trays with professional-grade whitening gels.
**Over-the-Counter (OTC) Products:** These include whitening toothpaste, strips, and gels. They are less potent than professional treatments and may take longer to show results.
Benefits of teeth whitening:
Improved Aesthetics: Whitening can remove stains and discoloration, enhancing the appearance of your teeth.
Boosted Confidence: A brighter smile often leads to increased self-confidence.
Non-Invasive: It’s a non-surgical and minimally invasive cosmetic dental procedure.
Risks and considerations:
Tooth Sensitivity: Whitening can cause temporary sensitivity to hot or cold foods and beverages.
Gum Irritation: Overuse or improper application of whitening products can irritate the gums.
Uneven Results: Whitening may not be equally effective on all teeth, leading to uneven results.
Duration of Effect: The duration of whitening effects varies; it may require touch-ups to maintain results.
Pre-existing Dental Issues: Whitening may not be suitable for everyone, especially those with dental restorations (crowns, fillings) as they do not respond to whitening treatments.
It’s crucial to consult with a dentist to discuss your specific needs and any potential risks associated with teeth whitening. They can help you choose the most appropriate and safe method for your situation.
Whitening Toothpastes; Facts and Fallacies
A Guide to Whitening Toothpastes in the UK: Efficacy Backed by Clinical Evidence
Whitening toothpastes are a popular choice for enhancing smiles, but how effective are they? In this blog, we’ll explore different types of whitening toothpastes available in the UK and evaluate their efficacy based on clinical evidence.
Abrasive-Based Whitening Toothpastes
These use mild abrasives like silica to remove surface stains caused by food, drinks, or smoking. While they can visibly improve brightness, clinical studies show they only remove extrinsic stains without altering the tooth’s natural color.
Efficacy: Effective for surface stain removal but not for deeper discoloration.
Enzyme-Based Whitening Toothpastes
Enzyme-based formulations (e.g., containing papain or bromelain) target protein pellicles that cause staining. Evidence suggests they can enhance stain removal without excessive abrasion, making them suitable for sensitive teeth.
Efficacy: Moderate improvement in surface brightness with minimal damage to enamel.
Peroxide-Based Whitening Toothpastes
Some toothpastes contain low levels of hydrogen or carbamide peroxide. Studies indicate they can help lighten intrinsic stains with consistent use over weeks. However, their whitening effect is less significant compared to professional bleaching.
Efficacy: Proven for mild intrinsic whitening, though results are subtle.
Charcoal Whitening Toothpastes
Charcoal-based products are widely marketed for whitening, but clinical evidence shows limited efficacy in removing stains. Excessive use may even harm enamel and gums due to high abrasiveness.
Efficacy: Poor stain removal with potential enamel damage.
Blue Covarine-Infused Toothpastes
These provide an immediate optical effect by depositing a blue pigment on teeth, creating the illusion of whiteness. While the results are temporary, studies support their effectiveness for a quick enhancement.
Efficacy: Temporary improvement in tooth brightness, ideal for short-term use.
Key Takeaways
Best for Surface Stains: Abrasive or enzyme-based toothpastes.
For Intrinsic Whitening: Peroxide-based formulas are most effective but offer mild results.
Quick Fix: Blue covarine toothpastes.
Avoid Overuse: Charcoal toothpastes due to abrasiveness.
For significant whitening or intrinsic stains, professional treatments remain the gold standard. Always consult your dentist to ensure the safest and most effective solution for your smile.
Dental Care and Coronavirus (COVID-19)
It is likely that the coronavirus will have an effect on your dental care.
Routine dental check-ups have been cancelled, and ongoing treatment plans may be disrupted. Where and how you access emergency dental treatment could also change.
This page includes advice on how you can access dental care, treatment and advice during the coronavirus pandemic.
Visiting the dental practice
If you are suffering with your oral health and need support, we are here to help.
To help stop the spread of coronavirus, we are advising against all routine and non-urgent dental treatment.
This includes:
Dental check-ups.
Preventive treatments such as scale and polish and fluoride varnishes.
Examinations and x-rays.
Appointments for braces.
Cosmetic dental treatment of any kind e.g. tooth whitening.
Routine denture treatment.
Treatments on teeth that are not painful e.g. fillings and extractions.
It is likely that your dental practice will contact you to postpone these appointments. If you do not hear from your dental practice, we recommend that you contact them to cancel your appointment and rearrange it for a later date.
In accordance to the instructions received by Public Health England (PHE) and CQC, all dental practices in England have temporarily ceased routine and non-urgent dental treatment. For emergency and urgent dental treatment, the dental surgery will provide remote (telephone or video-link) advice and assessment for further referral to the dedicated NHS Urgent Dental Care Centres (UDC) if necessary.
Whenever possible, stay at home and help stop the spread of coronavirus. This includes people of all ages – even if you do not have any symptoms or other health conditions.
Non-necessary dental treatment is not a reason for you to leave the home.
Urgent Dental Care
The NHS England has set up dedicated Urgent Dental Care Centres (UDC) for emergency and urgent dental conditions. Please note that this is not a walk-in service and requires appropriate referral by your dentist following remote triage.
If you are in pain, bleeding, swelling, or have had an accident and need urgent dental care, please contact your dental practice.
Please do not visit your dental practice without calling them first.
If you are not registered with any dental practice, please call 111 for further advice.
Dental Treatments in hospitals and A&E
To support NHS services and protect vital resources, it is important that you do not visit hospitals or A&E departments with dental problems.
If you need urgent or emergency dental treatment, contact your dental practice and they will be able to triage and direct you.
Dental care for vulnerable people and those with symptoms
If you need urgent dental care and are self-isolating because you have symptoms relating to coronavirus, or are a vulnerable person at higher risk, call NHS 111 or your dental practice.
The dental practice will be able to assess your needs and if necessary refer you to a special team/centre who will be able to treat you.
Buying oral health products
There is no shortage of oral health products like toothbrushes, toothpaste and mouthwash. Because of this, there is no need to stockpile them.
It is important to only buy what you need, when you need it.
Supermarkets remain open for essential food shopping and we advise that you buy any oral health products you need during this time. Please remember however to keep to social distancing rules and maintain two metres away from other shoppers.
When possible, instead of visiting supermarkets, we recommend that you buy oral health products online and have them delivered to your home.
Tips for good oral health
To help prevent dental problems from happening during coronavirus, here are some top tips for good oral health.
- Brush your teeth for two minutes, twice a day with a fluoride toothpaste.
- Do not share your toothbrushes. Keep the toothbrush clean and replace them frequently.
- The best time to brush is first thing in the morning and last thing at night before you go to bed.
- Cut down on how much sugar you have and how often you have it. This is even more important for children at home with increased temptation to snack and consume high sugar diet.
- Keep sugar consumption to mealtimes. This will reduce the time your teeth are under acid -attack.
- Maintain good hydration and avoid smoking and excessive consumption of alcohol.
- Use interdental brushes or floss to clean in between the teeth.
- Use non-alcohol based mouthwash daily to remove bad bacteria and keep fresh breath.
- Sugar-free chewing gum can help produce saliva and neutralise the plaque acids in your mouth.
More information and advice
Children coronavirus fact sheet, click here
For information about the coronavirus (COVID-19), please visit www.nhs.uk/conditions/coronavirus-covid-19/
The desire for the perfect Hollywood smile but at what cost?!

Cosmetic dentistry has become increasingly popular, largely as a result of social trends and increased media coverage. With the reality TV stars setting the trend in an industry now worth £2 billion, this understandable desire for the alleged ‘perfect smile’ needs to be tempered with an appropriate awareness of the significant risks associated with invasive cosmetic procedures such as veneers and crowns.
Patients need to be properly informed that elective removal of healthy enamel and dentine can result in pulpal injury and poorer periodontal health in the longer term, particularly if they are young. The duty of candour means that they ought to be informed that aggressive reduction of sound tooth tissue is not biologically neutral and results in structural weakening of their teeth. Less invasive procedures such as bleaching on its own or for example, combined with direct resin composite bonding, can satisfy many patient’s demands, while still being kinder to teeth and having much better fall-back positions for their future requirements.
It is the opinion of the British Endodontic Society, British Society for Restorative Dentistry, Restorative Dentistry UK, Dental Trauma UK, British Society of Prosthodontics and the British Society of Paediatric Dentistry that elective invasive cosmetic dental treatments can result in great benefit to patients, but that some aggressive treatments used to achieve them can produce significant morbidities in teeth which were previously healthy. This is a worrying and growing problem with many ethical, legal and biologic aspects, but many adverse outcomes for patients who request cosmetic dental improvements are preventable by using biologically safer initial approaches to treatment planning and its provision.
Dedicated personal, specialist care
The Specialist Dental Practice is the leading specialist restorative and implant dental practice in the county and has been setting the standards of specialist dentistry over the last 25 years.
The practice was established in 1973 and is conveniently located in the heart of Weybridge, Surrey. We are UK qualified and registered multi-specialist team offering specialist dental care of the highest quality and precision for the complex reconstruction cases involving dental implant therapy, gum disease treatment, root canal treatment, restoration of mutilated dentition and addressing challenges associated with partial and complete removable dentures.
We are delighted to welcome new referrals to our practice from both patients as well as professional colleagues.
Dental Implants
Essential questions to ask your dentist on dental implants
Taking the decision to have dental implants treatment is something most people will wish to consider quite carefully. Although this treatment can be an excellent long-term solution, it isn’t right for everybody and it is important to have a good understanding of exactly what is required. We have outlined a few essential questions and points you should be aware of before making your final decision.
WHAT ARE YOUR QUALIFICATIONS AND EXPERIENCE IN PLACING DENTAL IMPLANTS?
This is the most important question to ask and should be top of your list. Some clinicians have minimal training in placing dental implants and may only carry out this type of surgery a few times a year.
Our specialist care is based on dental specialties that are officially recognised by the General Dental Council UK. All accredited dental specialists are listed on the General Dental Council website www.gdc-uk.org. The specialist lists exist to:
• ensure high standards of training and assessment qualifying dentists to use a specialist title;
• indicate those dentists who possess recognised specialist knowledge, skills and attitudes;
• protect patients against unwarranted claims to be a specialist;
• facilitate appropriate referrals of patients;
• promote high standards of care by dentists qualified to use a specialist title; and
• encourage postgraduate education.
This list helps patients make an informed decision when they are looking for appropriately trained dentists to manage their dental care.
WHICH IMPLANT SYSTEMS DO YOU USE?
There are a few major dental implant companies that produce high-quality dental implants backed by years of research. These companies are well-known and well respected within the dental industry. There are numerous other companies that produce generic dental implants.
While these may still be of an acceptable quality, they lack the provenance of more widely known dental implant systems. There is another benefit of choosing dental implants made by one of the major companies as these implants are used worldwide. When you need an implant repaired or a component replaced or maintained, it is much easier to find a dentist willing to do this for you, no matter where you are in the world.
DO YOU PROVIDE COMPUTER GUIDED DENTAL IMPLANTS?
Computer guided dental implants surgery involves precisely planning using advanced diagnostics that include a cone beam CT scan and planning software. Once everything is planned, this computerised information is used to create a surgical guide or stent which allows precise placement of each implant.
We prefer to execute guided surgery where possible as it ensures your implant surgery is smoother, quicker and ultimately more comfortable and successful. Not all dentists will use this technique, but it is especially important when placing multiple implants where precision placement is even more vital.
Research shows that appropriately and precisely placed dental implants are less likely to have any problems and complications.
WILL IMPLANT SURGERY HURT?
You should not feel any pain during surgery based on effective local anaesthesia. We know many patients feel anxious at the thought of any oral surgery and if this applies to you then we can discuss additional sedation.
Our dental team is also very experienced at helping nervous patients feel at ease. Most of our patients will report no or very minimal discomfort that is very well managed with simple painkillers following implant surgery.
WILL I NEED A LONG TIME TO RECOVER AFTER IMPLANT SURGERY?
If you need just a single dental implant, you should be back to work the very next day. If you have multiple dental implants you might need a bit longer to recover; your dental implant dentist can give you more advice based on your situation.
Although you may feel some minor discomfort once the anaesthesia wears off, it is not uncommon to feel perfectly fine, especially after single dental implant placements. Again, this is something that can be discussed during your first consultation as it will depend on your treatment.
HOW LONG WILL IT TAKE TO COMPLETE IMPLANT TREATMENT?
Dental implant treatment can take up to several months to complete, as the surgery must be planned and once in place the implants need time to heal. It generally takes about 8-12 weeks for the dental implants to fully heal and to integrate with your jawbone, and the crown or bridge can be placed shortly after. Treatment may take slightly longer if you need bone grafts or tissue regeneration.
WILL I BE LEFT WITHOUT TEETH DURING IMPLANT HEALING?
This is a major concern for many people but there is no need to worry as temporary teeth can be provided while your implants heal. These temporary restorations can be fabricated before your implant surgery and may be placed immediately after surgery is completed.
WILL MY NEW IMPLANT TEETH LOOK NATURAL?
It is essential that your dental implants are placed in precisely the right position for the best functional and aesthetic effects. Here, at The Specialist dental Practice, our team are specialists in restoring and replacing missing teeth with crowns, bridges and dentures to the highest standards ensuring your new teeth are designed to look and feel wonderful. We also offer aftercare and advice on how to keep your implants clean.
HOW CAN I STOP MY DENTAL IMPLANTS FROM FAILING?
While some implants will fail naturally, a large part of implant success comes down to two factors:
• How well the implant is placed and the correct positioning in the jaw
• How well the implant is cared for after placement
Choosing a qualified and skilled implant dentist who is able to plan the correct positioning for your dental implants is key. Whilst you may think a general dentist is slightly cheaper, you may end up paying more in the future with implants that have not been placed correctly with significant potential complications.
The biggest misconception from dental implant patients is that once your dental implants are placed they will be there for life and are indestructible. The fact is, you will need to take care of your dental implants and make sure you regularly attend check-ups and clean your implants properly. Without this, your implants will have a larger chance of failing, both in a biologic and hardware sense.
SHOULD I GO ABROAD TO HAVE DENTAL IMPLANTS?
Dental tourism’ is a concept that has become increasingly popular over the last decade. Patients seek out dental treatment such as dental implants abroad and travel for the sole purpose of receiving cosmetic and restorative dentistry. The main attraction for patients is the cost of treatment in some other countries – it can look like prices are significantly cheaper, depending on the individual treatments. However, as with many things in life, what looks too good to be true often is. There are all kinds of hidden costs with choosing to get dental implants abroad including the prohibitive costs to fix a failing dental implant placed abroad, variation in the standard of care, and lack of long- term aftercare and maintenance plan.
Should you wish to seek more information on dental implant therapy, please contact the practice on 01932857585 or get in touch online info@weybridgedentist.co.uk to arrange for a consultation. In that way, we can assess for your individual needs and provide you with a customised treatment plan .
Specialist treatment for gum disease affecting teeth and dental implants

Understanding the importance of gum health
Gum disease affects many aspects of our life but is often overlooked as it has few symptoms in its early stages – that’s why it is often called ‘the silent disease’.
The vital thing about gum disease is that it is highly preventable and, especially in the early stages, quite easily treatable. Many studies link oral health to a number of significant conditions. There is strong evidence of the links between diabetes and gum disease. For Alzheimer’s and cardio health the role of gum disease is less clear. More than 45% of adults in the UK are affected by gum disease and, even at its most mild level, it can affect your quality of life.
Gum disease can affect dental implants as much as natural teeth. If you have any concerns about your dentition, speak to us and we will be happy to work with your dentist in managing your case.
Saving Your Natural Tooth
Specialist Endodontic Treatment
Nothing looks, feels or functions like your natural teeth, and endodontists are the experts in saving teeth. Keep smiling and eating the foods you love with endodontic treatment that can relieve your pain and save your teeth.
Sometimes your teeth may have infection or disease and will need additional care. When possible, you should always consider treatments to save your teeth. You may think, why not have a tooth pulled, especially if no one can see it, but you will know your tooth is missing and it will negatively impact your quality of life.
Don’t get a tooth pulled because you think its easier or more cost-effective. Missing teeth can cause other teeth to shift, affect your ability to properly chew and ruin your smile. Tooth extraction often is more painful than the infection itself, and replacing an extracted tooth with an artificial one requires additional dental visits that can quickly add up.
Modern endodontics offers advancements in technologies, procedures and materials, giving you many treatment options to save your natural teeth. It’s important to understand your choices and how they’ll impact both your tooth and your future dental health. It’s always best to retain your natural teeth whenever possible and endodontic treatment should be your first choice for the best health and cosmetic results. Endodontists are specialists in saving teeth. They can evaluate your condition and provide the best treatment plan to help you save your teeth for a lifetime.
Here are some tips for saving your teeth:
- When given a choice between tooth extraction and root canal treatment, always opt for a root canal. No denture, bridge or implant will look, feel and function as well as a natural tooth.
- Act immediately when you experience symptoms of swelling or pain. Most endodontists can accommodate emergency cases, even on weekends, ensuring you’ll be seen quickly.
- If your dentist recommends tooth extraction, ask whether the root canal is an option.If you’re told root canal is not an option, ask why and request a referral to an endodontist.
Root canal treatment from an endodontist is virtually painless and often leaves you with less discomfort during recovery than if you have your natural tooth extracted. Thanks to modern techniques and effective anesthesia, patients who experience root canals are six times more likely to describe it as painless than patients who have a tooth extracted! Take the time to learn more about root canal treatment and some of the common misconceptions about it and then take the first step to a pain-free, healthy mouth by visiting an endodontist.
How does endodontic treatment save the tooth?
It’s necessary to have endodontic or root canal treatment when the inside of your tooth (the pulp) becomes inflamed or infected as a result of deep decay, repeated dental procedures, faulty crowns or a crack or chip in the tooth. Trauma to your tooth may also cause pulp damage even if the tooth has no visible chips or cracks. If pulp inflammation or infection is left untreated, it can cause pain or lead to an abscess.
When you undergo a root canal or other endodontic treatment, the inflamed or infected pulp is removed and the inside of the tooth is carefully cleaned and disinfected, then filled and sealed with a rubber-like material called gutta-percha. Afterward, the tooth is restored with a crown or filling for protection and will continue to function like any other tooth.
Endodontic treatment helps you maintain your natural smile, continue eating the foods you love and limits the need for ongoing dental work. With proper care, most teeth that have had root canal treatment can last a lifetime.
For more detailed information on root canal or to organise for a consultation, call us or get in touch online.
Biomimetic Dentistry
What is Biomimetic Dentistry?

Translated literally, biomimetic dentistry means to copy what is life-like. Nature has provided the most successful and ideal properties to our natural teeth. When restoring damaged, broken, and decayed teeth, the goal is to return the tooth to its original strength, function, and esthetics. Biomimetic dentistry accomplishes all of this in a conservative, strong, and attractive approach.
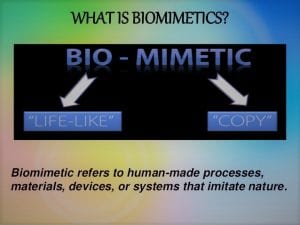
Why is it so important?
Tooth preservation and dental conservation lie at the heart of biomimetic dentistry.
Biomimetic dentistry replicates the strength, function, and aesthetics of natural teeth by replacing only damaged, decayed, and broken tooth structure. The principle employs techniques and materials that provide a perfect balance of nature, art and science.
Teeth move, bend and have physical dynamics of force that must be accounted for while re-making the tooth with nature as our guide. Much of the amputation of tooth structure can be eliminated with modern science. We can say that tooth preservation and dental conservation lie at the heart of biomimetic dentistry.
The economic implications of not needing the advanced, invasive care seen in traditional (amputational) dentistry have profound positive effects on people’s lives. We can now help patients create healthy and happy mouths with simple, and often painless techniques!
Patients are happier and often spend less compared to conventional treatment.
Give us a call to find out more or book a consultation appointment.
Want to stop snoring?
As a condition that affects over 40% of the population, it is no surprise that the majority of us have been impacted by snoring in some way, shape or form. There are both varying degrees and varying types of snoring: it can be ‘simple’, or it can be symptomatic and may require further exploration. Regardless, there are a number of conditions associated, including:
- diminished energy
- lack of concentration
- increased risk of stress
- reduced libido
- high blood pressure
As well as the impact to the snorer, a lack of sleep on the bed partner’s behalf is also dangerous for their health and well-being. Many cases are reported by the bed-partner, with the snorer having very little awareness of their bedtime activities.

Thankfully, there are many interventions that can assist with snoring. Before discussing these, however, it is first important to highlight the cause.
What causes snoring?
Once we are asleep, our muscles relax. This can result in the soft tissues in the throat vibrating, causing the familiar snoring sound.
However, this doesn’t happen to everyone: there are a number of factors that can increase chances of snoring, including: obesity, gender, age, alcohol, and medication. For most sufferers, snoring occurs in isolation (simple snoring). In these cases, it is often the bed-partner that suffers, with the snorer unaware that they are causing such a disturbance. However, it can also take place as part of a more serious condition, obstructive sleep apnoea, which can be potentially life-threatening if not treated correctly.
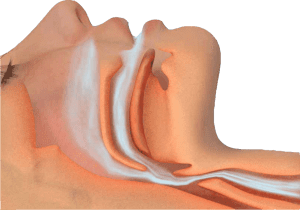
What is obstructive sleep apnoea (OSA)?
OSA is a serious condition where, for short periods of time, the airway becomes blocked during sleep, cutting off oxygen reaching the lungs. There are two types of breathing disruption associated with OSA:
- Apnoea – where the muscles collapse sufficiently enough to cause a total blockage of the airway for 10 seconds or more
- Hypopnoea – partial blockage of the airway that causes an airflow reduction of more than 50% for 10 seconds or more
Both of these problems can occur several times throughout the night and are most commonly recognised by loud snoring, paired with snorts, gasps, or laboured breathing. This leads to disruption for both the bed-partner AND the sufferer, with the snorer often waking feeling tired due to a night with reduced oxygen intake.
There are many associations with obstructive sleep apnoea, and, due to fat distribution, middle-aged males are twice as likely to suffer from OSA in comparison to middle-aged females. The discrepancy does start to level out, however, believed to be due to hormonal changes after menopause.
What are the treatments for snoring?
Though many snorers and tired bed-partners typically look to their doctor for help when it comes to snoring, their dentist arguably has a larger part to play – initially at least.
As snoring is typically caused by the lower jaw dropping back during sleep, the easiest way to stop it is to prevent the jaw from slipping backwards. This can be achieved with a device called a Mandibular Advancement Splint (MAS). Available from trained dentists, there are a number of devices available, one of which is the Sleepwell.

The most clinically proven MAS for the treatment of snoring & mild to moderate sleep apnoea, the Sleepwell is a two-piece device that is fully-adjustable by the wearer, and designed to hold your lower jaw forward. Holistically, however, there may be other behaviours that could assist with the problem, such as:
- Sleeping position – lying on your back inevitably is the worst position for snoring. Trying different positions may have a positive effect.
- Bed-time ‘hygiene’ – avoiding alcohol or caffeine in the evenings can help. Both muscle relaxants, they can increase the chances of snoring.
- Weight-loss – holding excess fat around your neck can play a major role in both snoring and sleep apnoea.
National Stop Snoring Week 23-27 April 2018
Cosmetic Dentistry- What You Should Know

Cosmetic dentistry has become increasingly popular, largely as a result of social trends and increased media coverage. This understandable desire for the alleged ‘perfect smile’ needs to be tempered with an appropriate awareness of the significant risks associated with invasive cosmetic procedures such as veneers and crowns. Patients need to be properly informed that elective removal of healthy enamel and dentine can result in pulpal injury and poorer periodontal health in the longer term, particularly if they are young. The duty of candour means that they ought to be informed that aggressive reduction of sound tooth tissue is not biologically neutral and results in structural weakening of their teeth. Less invasive procedures such as bleaching on its own or for example, combined with direct resin composite bonding, can satisfy many patient’s demands, while still being kinder to teeth and having much better fall-back positions for their future requirements. It is the opinion of the British Endodontic Society, British Society for Restorative Dentistry, Restorative Dentistry UK, Dental Trauma UK, British Society of Prosthodontics and the British Society of Paediatric Dentistry that elective invasive cosmetic dental treatments can result in great benefit to patients, but that some aggressive treatments used to achieve them can produce significant morbidities in teeth which were previously healthy. This is a worrying and growing problem with many ethical, legal and biologic aspects, but many adverse outcomes for patients who request cosmetic dental improvements are preventable by using biologically safer initial approaches to treatment planning and its provision.
Mouth Cancer Awareness Month

Most people have heard of cancer affecting parts of the body such as the lungs or breasts. However, cancer can also occur in the mouth, where the disease can affect the lips, tongue, cheeks and throat.
Anyone can be affected by mouth cancer, whether they have their own teeth or not. Mouth cancers are more common in people over 40, particularly men. However, research has shown that mouth cancer is becoming more common in younger patients and in women. In the last year more than 7,000 have been diagnosed with mouth cancer in the UK – an increase of more than a third compared to a decade ago.
Sadly, more than 1,800 people in the UK lose their life to mouth cancer every year. Many of these deaths could be prevented if the cancer was caught early enough. As it is, people with mouth cancer are more likely to die than those having cervical cancer or melanoma skin cancer.
Find out more at http://www.mouthcancer.org
Teeth whitening
Teeth whitening can be safe when done under the guidance of a dental professional or by following the instructions of over-the-counter products. However, it’s important to be aware of potential side effects, such as tooth sensitivity or gum irritation. Consult your dentist to discuss the best and safest whitening options for your specific needs.
Methods of teeth whitening:
**Professional Whitening:**This is done by a dentist and is the most effective method. It can involve in-office treatments using strong bleaching agents or custom-fitted trays with professional-grade whitening gels.
**Over-the-Counter (OTC) Products:** These include whitening toothpaste, strips, and gels. They are less potent than professional treatments and may take longer to show results.
Benefits of teeth whitening:
Improved Aesthetics: Whitening can remove stains and discoloration, enhancing the appearance of your teeth.
Boosted Confidence: A brighter smile often leads to increased self-confidence.
Non-Invasive: It’s a non-surgical and minimally invasive cosmetic dental procedure.
Risks and considerations:
Tooth Sensitivity: Whitening can cause temporary sensitivity to hot or cold foods and beverages.
Gum Irritation: Overuse or improper application of whitening products can irritate the gums.
Uneven Results: Whitening may not be equally effective on all teeth, leading to uneven results.
Duration of Effect: The duration of whitening effects varies; it may require touch-ups to maintain results.
Pre-existing Dental Issues: Whitening may not be suitable for everyone, especially those with dental restorations (crowns, fillings) as they do not respond to whitening treatments.
It’s crucial to consult with a dentist to discuss your specific needs and any potential risks associated with teeth whitening. They can help you choose the most appropriate and safe method for your situation.
Whitening Toothpastes; Facts and Fallacies
A Guide to Whitening Toothpastes in the UK: Efficacy Backed by Clinical Evidence
Whitening toothpastes are a popular choice for enhancing smiles, but how effective are they? In this blog, we’ll explore different types of whitening toothpastes available in the UK and evaluate their efficacy based on clinical evidence.
Abrasive-Based Whitening Toothpastes
These use mild abrasives like silica to remove surface stains caused by food, drinks, or smoking. While they can visibly improve brightness, clinical studies show they only remove extrinsic stains without altering the tooth’s natural color.
Efficacy: Effective for surface stain removal but not for deeper discoloration.
Enzyme-Based Whitening Toothpastes
Enzyme-based formulations (e.g., containing papain or bromelain) target protein pellicles that cause staining. Evidence suggests they can enhance stain removal without excessive abrasion, making them suitable for sensitive teeth.
Efficacy: Moderate improvement in surface brightness with minimal damage to enamel.
Peroxide-Based Whitening Toothpastes
Some toothpastes contain low levels of hydrogen or carbamide peroxide. Studies indicate they can help lighten intrinsic stains with consistent use over weeks. However, their whitening effect is less significant compared to professional bleaching.
Efficacy: Proven for mild intrinsic whitening, though results are subtle.
Charcoal Whitening Toothpastes
Charcoal-based products are widely marketed for whitening, but clinical evidence shows limited efficacy in removing stains. Excessive use may even harm enamel and gums due to high abrasiveness.
Efficacy: Poor stain removal with potential enamel damage.
Blue Covarine-Infused Toothpastes
These provide an immediate optical effect by depositing a blue pigment on teeth, creating the illusion of whiteness. While the results are temporary, studies support their effectiveness for a quick enhancement.
Efficacy: Temporary improvement in tooth brightness, ideal for short-term use.
Key Takeaways
Best for Surface Stains: Abrasive or enzyme-based toothpastes.
For Intrinsic Whitening: Peroxide-based formulas are most effective but offer mild results.
Quick Fix: Blue covarine toothpastes.
Avoid Overuse: Charcoal toothpastes due to abrasiveness.
For significant whitening or intrinsic stains, professional treatments remain the gold standard. Always consult your dentist to ensure the safest and most effective solution for your smile.
Dental Care and Coronavirus (COVID-19)
It is likely that the coronavirus will have an effect on your dental care.
Routine dental check-ups have been cancelled, and ongoing treatment plans may be disrupted. Where and how you access emergency dental treatment could also change.
This page includes advice on how you can access dental care, treatment and advice during the coronavirus pandemic.
Visiting the dental practice
If you are suffering with your oral health and need support, we are here to help.
To help stop the spread of coronavirus, we are advising against all routine and non-urgent dental treatment.
This includes:
Dental check-ups.
Preventive treatments such as scale and polish and fluoride varnishes.
Examinations and x-rays.
Appointments for braces.
Cosmetic dental treatment of any kind e.g. tooth whitening.
Routine denture treatment.
Treatments on teeth that are not painful e.g. fillings and extractions.
It is likely that your dental practice will contact you to postpone these appointments. If you do not hear from your dental practice, we recommend that you contact them to cancel your appointment and rearrange it for a later date.
In accordance to the instructions received by Public Health England (PHE) and CQC, all dental practices in England have temporarily ceased routine and non-urgent dental treatment. For emergency and urgent dental treatment, the dental surgery will provide remote (telephone or video-link) advice and assessment for further referral to the dedicated NHS Urgent Dental Care Centres (UDC) if necessary.
Whenever possible, stay at home and help stop the spread of coronavirus. This includes people of all ages – even if you do not have any symptoms or other health conditions.
Non-necessary dental treatment is not a reason for you to leave the home.
Urgent Dental Care
The NHS England has set up dedicated Urgent Dental Care Centres (UDC) for emergency and urgent dental conditions. Please note that this is not a walk-in service and requires appropriate referral by your dentist following remote triage.
If you are in pain, bleeding, swelling, or have had an accident and need urgent dental care, please contact your dental practice.
Please do not visit your dental practice without calling them first.
If you are not registered with any dental practice, please call 111 for further advice.
Dental Treatments in hospitals and A&E
To support NHS services and protect vital resources, it is important that you do not visit hospitals or A&E departments with dental problems.
If you need urgent or emergency dental treatment, contact your dental practice and they will be able to triage and direct you.
Dental care for vulnerable people and those with symptoms
If you need urgent dental care and are self-isolating because you have symptoms relating to coronavirus, or are a vulnerable person at higher risk, call NHS 111 or your dental practice.
The dental practice will be able to assess your needs and if necessary refer you to a special team/centre who will be able to treat you.
Buying oral health products
There is no shortage of oral health products like toothbrushes, toothpaste and mouthwash. Because of this, there is no need to stockpile them.
It is important to only buy what you need, when you need it.
Supermarkets remain open for essential food shopping and we advise that you buy any oral health products you need during this time. Please remember however to keep to social distancing rules and maintain two metres away from other shoppers.
When possible, instead of visiting supermarkets, we recommend that you buy oral health products online and have them delivered to your home.
Tips for good oral health
To help prevent dental problems from happening during coronavirus, here are some top tips for good oral health.
- Brush your teeth for two minutes, twice a day with a fluoride toothpaste.
- Do not share your toothbrushes. Keep the toothbrush clean and replace them frequently.
- The best time to brush is first thing in the morning and last thing at night before you go to bed.
- Cut down on how much sugar you have and how often you have it. This is even more important for children at home with increased temptation to snack and consume high sugar diet.
- Keep sugar consumption to mealtimes. This will reduce the time your teeth are under acid -attack.
- Maintain good hydration and avoid smoking and excessive consumption of alcohol.
- Use interdental brushes or floss to clean in between the teeth.
- Use non-alcohol based mouthwash daily to remove bad bacteria and keep fresh breath.
- Sugar-free chewing gum can help produce saliva and neutralise the plaque acids in your mouth.
More information and advice
Children coronavirus fact sheet, click here
For information about the coronavirus (COVID-19), please visit www.nhs.uk/conditions/coronavirus-covid-19/
The desire for the perfect Hollywood smile but at what cost?!

Cosmetic dentistry has become increasingly popular, largely as a result of social trends and increased media coverage. With the reality TV stars setting the trend in an industry now worth £2 billion, this understandable desire for the alleged ‘perfect smile’ needs to be tempered with an appropriate awareness of the significant risks associated with invasive cosmetic procedures such as veneers and crowns.
Patients need to be properly informed that elective removal of healthy enamel and dentine can result in pulpal injury and poorer periodontal health in the longer term, particularly if they are young. The duty of candour means that they ought to be informed that aggressive reduction of sound tooth tissue is not biologically neutral and results in structural weakening of their teeth. Less invasive procedures such as bleaching on its own or for example, combined with direct resin composite bonding, can satisfy many patient’s demands, while still being kinder to teeth and having much better fall-back positions for their future requirements.
It is the opinion of the British Endodontic Society, British Society for Restorative Dentistry, Restorative Dentistry UK, Dental Trauma UK, British Society of Prosthodontics and the British Society of Paediatric Dentistry that elective invasive cosmetic dental treatments can result in great benefit to patients, but that some aggressive treatments used to achieve them can produce significant morbidities in teeth which were previously healthy. This is a worrying and growing problem with many ethical, legal and biologic aspects, but many adverse outcomes for patients who request cosmetic dental improvements are preventable by using biologically safer initial approaches to treatment planning and its provision.
Dedicated personal, specialist care
The Specialist Dental Practice is the leading specialist restorative and implant dental practice in the county and has been setting the standards of specialist dentistry over the last 25 years.
The practice was established in 1973 and is conveniently located in the heart of Weybridge, Surrey. We are UK qualified and registered multi-specialist team offering specialist dental care of the highest quality and precision for the complex reconstruction cases involving dental implant therapy, gum disease treatment, root canal treatment, restoration of mutilated dentition and addressing challenges associated with partial and complete removable dentures.
We are delighted to welcome new referrals to our practice from both patients as well as professional colleagues.
Dental Implants
Essential questions to ask your dentist on dental implants
Taking the decision to have dental implants treatment is something most people will wish to consider quite carefully. Although this treatment can be an excellent long-term solution, it isn’t right for everybody and it is important to have a good understanding of exactly what is required. We have outlined a few essential questions and points you should be aware of before making your final decision.
WHAT ARE YOUR QUALIFICATIONS AND EXPERIENCE IN PLACING DENTAL IMPLANTS?
This is the most important question to ask and should be top of your list. Some clinicians have minimal training in placing dental implants and may only carry out this type of surgery a few times a year.
Our specialist care is based on dental specialties that are officially recognised by the General Dental Council UK. All accredited dental specialists are listed on the General Dental Council website www.gdc-uk.org. The specialist lists exist to:
• ensure high standards of training and assessment qualifying dentists to use a specialist title;
• indicate those dentists who possess recognised specialist knowledge, skills and attitudes;
• protect patients against unwarranted claims to be a specialist;
• facilitate appropriate referrals of patients;
• promote high standards of care by dentists qualified to use a specialist title; and
• encourage postgraduate education.
This list helps patients make an informed decision when they are looking for appropriately trained dentists to manage their dental care.
WHICH IMPLANT SYSTEMS DO YOU USE?
There are a few major dental implant companies that produce high-quality dental implants backed by years of research. These companies are well-known and well respected within the dental industry. There are numerous other companies that produce generic dental implants.
While these may still be of an acceptable quality, they lack the provenance of more widely known dental implant systems. There is another benefit of choosing dental implants made by one of the major companies as these implants are used worldwide. When you need an implant repaired or a component replaced or maintained, it is much easier to find a dentist willing to do this for you, no matter where you are in the world.
DO YOU PROVIDE COMPUTER GUIDED DENTAL IMPLANTS?
Computer guided dental implants surgery involves precisely planning using advanced diagnostics that include a cone beam CT scan and planning software. Once everything is planned, this computerised information is used to create a surgical guide or stent which allows precise placement of each implant.
We prefer to execute guided surgery where possible as it ensures your implant surgery is smoother, quicker and ultimately more comfortable and successful. Not all dentists will use this technique, but it is especially important when placing multiple implants where precision placement is even more vital.
Research shows that appropriately and precisely placed dental implants are less likely to have any problems and complications.
WILL IMPLANT SURGERY HURT?
You should not feel any pain during surgery based on effective local anaesthesia. We know many patients feel anxious at the thought of any oral surgery and if this applies to you then we can discuss additional sedation.
Our dental team is also very experienced at helping nervous patients feel at ease. Most of our patients will report no or very minimal discomfort that is very well managed with simple painkillers following implant surgery.
WILL I NEED A LONG TIME TO RECOVER AFTER IMPLANT SURGERY?
If you need just a single dental implant, you should be back to work the very next day. If you have multiple dental implants you might need a bit longer to recover; your dental implant dentist can give you more advice based on your situation.
Although you may feel some minor discomfort once the anaesthesia wears off, it is not uncommon to feel perfectly fine, especially after single dental implant placements. Again, this is something that can be discussed during your first consultation as it will depend on your treatment.
HOW LONG WILL IT TAKE TO COMPLETE IMPLANT TREATMENT?
Dental implant treatment can take up to several months to complete, as the surgery must be planned and once in place the implants need time to heal. It generally takes about 8-12 weeks for the dental implants to fully heal and to integrate with your jawbone, and the crown or bridge can be placed shortly after. Treatment may take slightly longer if you need bone grafts or tissue regeneration.
WILL I BE LEFT WITHOUT TEETH DURING IMPLANT HEALING?
This is a major concern for many people but there is no need to worry as temporary teeth can be provided while your implants heal. These temporary restorations can be fabricated before your implant surgery and may be placed immediately after surgery is completed.
WILL MY NEW IMPLANT TEETH LOOK NATURAL?
It is essential that your dental implants are placed in precisely the right position for the best functional and aesthetic effects. Here, at The Specialist dental Practice, our team are specialists in restoring and replacing missing teeth with crowns, bridges and dentures to the highest standards ensuring your new teeth are designed to look and feel wonderful. We also offer aftercare and advice on how to keep your implants clean.
HOW CAN I STOP MY DENTAL IMPLANTS FROM FAILING?
While some implants will fail naturally, a large part of implant success comes down to two factors:
• How well the implant is placed and the correct positioning in the jaw
• How well the implant is cared for after placement
Choosing a qualified and skilled implant dentist who is able to plan the correct positioning for your dental implants is key. Whilst you may think a general dentist is slightly cheaper, you may end up paying more in the future with implants that have not been placed correctly with significant potential complications.
The biggest misconception from dental implant patients is that once your dental implants are placed they will be there for life and are indestructible. The fact is, you will need to take care of your dental implants and make sure you regularly attend check-ups and clean your implants properly. Without this, your implants will have a larger chance of failing, both in a biologic and hardware sense.
SHOULD I GO ABROAD TO HAVE DENTAL IMPLANTS?
Dental tourism’ is a concept that has become increasingly popular over the last decade. Patients seek out dental treatment such as dental implants abroad and travel for the sole purpose of receiving cosmetic and restorative dentistry. The main attraction for patients is the cost of treatment in some other countries – it can look like prices are significantly cheaper, depending on the individual treatments. However, as with many things in life, what looks too good to be true often is. There are all kinds of hidden costs with choosing to get dental implants abroad including the prohibitive costs to fix a failing dental implant placed abroad, variation in the standard of care, and lack of long- term aftercare and maintenance plan.
Should you wish to seek more information on dental implant therapy, please contact the practice on 01932857585 or get in touch online info@weybridgedentist.co.uk to arrange for a consultation. In that way, we can assess for your individual needs and provide you with a customised treatment plan .
Specialist treatment for gum disease affecting teeth and dental implants

Understanding the importance of gum health
Gum disease affects many aspects of our life but is often overlooked as it has few symptoms in its early stages – that’s why it is often called ‘the silent disease’.
The vital thing about gum disease is that it is highly preventable and, especially in the early stages, quite easily treatable. Many studies link oral health to a number of significant conditions. There is strong evidence of the links between diabetes and gum disease. For Alzheimer’s and cardio health the role of gum disease is less clear. More than 45% of adults in the UK are affected by gum disease and, even at its most mild level, it can affect your quality of life.
Gum disease can affect dental implants as much as natural teeth. If you have any concerns about your dentition, speak to us and we will be happy to work with your dentist in managing your case.
Saving Your Natural Tooth
Specialist Endodontic Treatment
Nothing looks, feels or functions like your natural teeth, and endodontists are the experts in saving teeth. Keep smiling and eating the foods you love with endodontic treatment that can relieve your pain and save your teeth.
Sometimes your teeth may have infection or disease and will need additional care. When possible, you should always consider treatments to save your teeth. You may think, why not have a tooth pulled, especially if no one can see it, but you will know your tooth is missing and it will negatively impact your quality of life.
Don’t get a tooth pulled because you think its easier or more cost-effective. Missing teeth can cause other teeth to shift, affect your ability to properly chew and ruin your smile. Tooth extraction often is more painful than the infection itself, and replacing an extracted tooth with an artificial one requires additional dental visits that can quickly add up.
Modern endodontics offers advancements in technologies, procedures and materials, giving you many treatment options to save your natural teeth. It’s important to understand your choices and how they’ll impact both your tooth and your future dental health. It’s always best to retain your natural teeth whenever possible and endodontic treatment should be your first choice for the best health and cosmetic results. Endodontists are specialists in saving teeth. They can evaluate your condition and provide the best treatment plan to help you save your teeth for a lifetime.
Here are some tips for saving your teeth:
- When given a choice between tooth extraction and root canal treatment, always opt for a root canal. No denture, bridge or implant will look, feel and function as well as a natural tooth.
- Act immediately when you experience symptoms of swelling or pain. Most endodontists can accommodate emergency cases, even on weekends, ensuring you’ll be seen quickly.
- If your dentist recommends tooth extraction, ask whether the root canal is an option.If you’re told root canal is not an option, ask why and request a referral to an endodontist.
Root canal treatment from an endodontist is virtually painless and often leaves you with less discomfort during recovery than if you have your natural tooth extracted. Thanks to modern techniques and effective anesthesia, patients who experience root canals are six times more likely to describe it as painless than patients who have a tooth extracted! Take the time to learn more about root canal treatment and some of the common misconceptions about it and then take the first step to a pain-free, healthy mouth by visiting an endodontist.
How does endodontic treatment save the tooth?
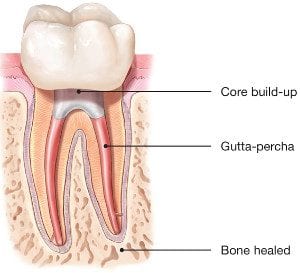
It’s necessary to have endodontic or root canal treatment when the inside of your tooth (the pulp) becomes inflamed or infected as a result of deep decay, repeated dental procedures, faulty crowns or a crack or chip in the tooth. Trauma to your tooth may also cause pulp damage even if the tooth has no visible chips or cracks. If pulp inflammation or infection is left untreated, it can cause pain or lead to an abscess.
When you undergo a root canal or other endodontic treatment, the inflamed or infected pulp is removed and the inside of the tooth is carefully cleaned and disinfected, then filled and sealed with a rubber-like material called gutta-percha. Afterward, the tooth is restored with a crown or filling for protection and will continue to function like any other tooth.
Endodontic treatment helps you maintain your natural smile, continue eating the foods you love and limits the need for ongoing dental work. With proper care, most teeth that have had root canal treatment can last a lifetime.
For more detailed information on root canal or to organise for a consultation, call us or get in touch online.
Biomimetic Dentistry
What is Biomimetic Dentistry?

Translated literally, biomimetic dentistry means to copy what is life-like. Nature has provided the most successful and ideal properties to our natural teeth. When restoring damaged, broken, and decayed teeth, the goal is to return the tooth to its original strength, function, and esthetics. Biomimetic dentistry accomplishes all of this in a conservative, strong, and attractive approach.
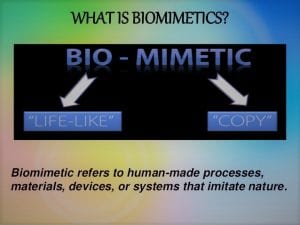
Why is it so important?
Tooth preservation and dental conservation lie at the heart of biomimetic dentistry.
Biomimetic dentistry replicates the strength, function, and aesthetics of natural teeth by replacing only damaged, decayed, and broken tooth structure. The principle employs techniques and materials that provide a perfect balance of nature, art and science.
Teeth move, bend and have physical dynamics of force that must be accounted for while re-making the tooth with nature as our guide. Much of the amputation of tooth structure can be eliminated with modern science. We can say that tooth preservation and dental conservation lie at the heart of biomimetic dentistry.
The economic implications of not needing the advanced, invasive care seen in traditional (amputational) dentistry have profound positive effects on people’s lives. We can now help patients create healthy and happy mouths with simple, and often painless techniques!
Patients are happier and often spend less compared to conventional treatment.
Give us a call to find out more or book a consultation appointment.
Want to stop snoring?
As a condition that affects over 40% of the population, it is no surprise that the majority of us have been impacted by snoring in some way, shape or form. There are both varying degrees and varying types of snoring: it can be ‘simple’, or it can be symptomatic and may require further exploration. Regardless, there are a number of conditions associated, including:
- diminished energy
- lack of concentration
- increased risk of stress
- reduced libido
- high blood pressure
As well as the impact to the snorer, a lack of sleep on the bed partner’s behalf is also dangerous for their health and well-being. Many cases are reported by the bed-partner, with the snorer having very little awareness of their bedtime activities.

Thankfully, there are many interventions that can assist with snoring. Before discussing these, however, it is first important to highlight the cause.
What causes snoring?
Once we are asleep, our muscles relax. This can result in the soft tissues in the throat vibrating, causing the familiar snoring sound.
However, this doesn’t happen to everyone: there are a number of factors that can increase chances of snoring, including: obesity, gender, age, alcohol, and medication. For most sufferers, snoring occurs in isolation (simple snoring). In these cases, it is often the bed-partner that suffers, with the snorer unaware that they are causing such a disturbance. However, it can also take place as part of a more serious condition, obstructive sleep apnoea, which can be potentially life-threatening if not treated correctly.
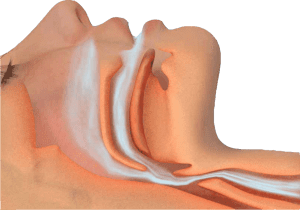
What is obstructive sleep apnoea (OSA)?
OSA is a serious condition where, for short periods of time, the airway becomes blocked during sleep, cutting off oxygen reaching the lungs. There are two types of breathing disruption associated with OSA:
- Apnoea – where the muscles collapse sufficiently enough to cause a total blockage of the airway for 10 seconds or more
- Hypopnoea – partial blockage of the airway that causes an airflow reduction of more than 50% for 10 seconds or more
Both of these problems can occur several times throughout the night and are most commonly recognised by loud snoring, paired with snorts, gasps, or laboured breathing. This leads to disruption for both the bed-partner AND the sufferer, with the snorer often waking feeling tired due to a night with reduced oxygen intake.
There are many associations with obstructive sleep apnoea, and, due to fat distribution, middle-aged males are twice as likely to suffer from OSA in comparison to middle-aged females. The discrepancy does start to level out, however, believed to be due to hormonal changes after menopause.
What are the treatments for snoring?
Though many snorers and tired bed-partners typically look to their doctor for help when it comes to snoring, their dentist arguably has a larger part to play – initially at least.
As snoring is typically caused by the lower jaw dropping back during sleep, the easiest way to stop it is to prevent the jaw from slipping backwards. This can be achieved with a device called a Mandibular Advancement Splint (MAS). Available from trained dentists, there are a number of devices available, one of which is the Sleepwell.

The most clinically proven MAS for the treatment of snoring & mild to moderate sleep apnoea, the Sleepwell is a two-piece device that is fully-adjustable by the wearer, and designed to hold your lower jaw forward. Holistically, however, there may be other behaviours that could assist with the problem, such as:
- Sleeping position – lying on your back inevitably is the worst position for snoring. Trying different positions may have a positive effect.
- Bed-time ‘hygiene’ – avoiding alcohol or caffeine in the evenings can help. Both muscle relaxants, they can increase the chances of snoring.
- Weight-loss – holding excess fat around your neck can play a major role in both snoring and sleep apnoea.
National Stop Snoring Week 23-27 April 2018
Cosmetic Dentistry- What You Should Know

Cosmetic dentistry has become increasingly popular, largely as a result of social trends and increased media coverage. This understandable desire for the alleged ‘perfect smile’ needs to be tempered with an appropriate awareness of the significant risks associated with invasive cosmetic procedures such as veneers and crowns. Patients need to be properly informed that elective removal of healthy enamel and dentine can result in pulpal injury and poorer periodontal health in the longer term, particularly if they are young. The duty of candour means that they ought to be informed that aggressive reduction of sound tooth tissue is not biologically neutral and results in structural weakening of their teeth. Less invasive procedures such as bleaching on its own or for example, combined with direct resin composite bonding, can satisfy many patient’s demands, while still being kinder to teeth and having much better fall-back positions for their future requirements. It is the opinion of the British Endodontic Society, British Society for Restorative Dentistry, Restorative Dentistry UK, Dental Trauma UK, British Society of Prosthodontics and the British Society of Paediatric Dentistry that elective invasive cosmetic dental treatments can result in great benefit to patients, but that some aggressive treatments used to achieve them can produce significant morbidities in teeth which were previously healthy. This is a worrying and growing problem with many ethical, legal and biologic aspects, but many adverse outcomes for patients who request cosmetic dental improvements are preventable by using biologically safer initial approaches to treatment planning and its provision.
Mouth Cancer Awareness Month

Most people have heard of cancer affecting parts of the body such as the lungs or breasts. However, cancer can also occur in the mouth, where the disease can affect the lips, tongue, cheeks and throat.
Anyone can be affected by mouth cancer, whether they have their own teeth or not. Mouth cancers are more common in people over 40, particularly men. However, research has shown that mouth cancer is becoming more common in younger patients and in women. In the last year more than 7,000 have been diagnosed with mouth cancer in the UK – an increase of more than a third compared to a decade ago.
Sadly, more than 1,800 people in the UK lose their life to mouth cancer every year. Many of these deaths could be prevented if the cancer was caught early enough. As it is, people with mouth cancer are more likely to die than those having cervical cancer or melanoma skin cancer.
Find out more at http://www.mouthcancer.org
Teeth whitening
Teeth whitening can be safe when done under the guidance of a dental professional or by following the instructions of over-the-counter products. However, it’s important to be aware of potential side effects, such as tooth sensitivity or gum irritation. Consult your dentist to discuss the best and safest whitening options for your specific needs.
Methods of teeth whitening:
**Professional Whitening:**This is done by a dentist and is the most effective method. It can involve in-office treatments using strong bleaching agents or custom-fitted trays with professional-grade whitening gels.
**Over-the-Counter (OTC) Products:** These include whitening toothpaste, strips, and gels. They are less potent than professional treatments and may take longer to show results.
Benefits of teeth whitening:
Improved Aesthetics: Whitening can remove stains and discoloration, enhancing the appearance of your teeth.
Boosted Confidence: A brighter smile often leads to increased self-confidence.
Non-Invasive: It’s a non-surgical and minimally invasive cosmetic dental procedure.
Risks and considerations:
Tooth Sensitivity: Whitening can cause temporary sensitivity to hot or cold foods and beverages.
Gum Irritation: Overuse or improper application of whitening products can irritate the gums.
Uneven Results: Whitening may not be equally effective on all teeth, leading to uneven results.
Duration of Effect: The duration of whitening effects varies; it may require touch-ups to maintain results.
Pre-existing Dental Issues: Whitening may not be suitable for everyone, especially those with dental restorations (crowns, fillings) as they do not respond to whitening treatments.
It’s crucial to consult with a dentist to discuss your specific needs and any potential risks associated with teeth whitening. They can help you choose the most appropriate and safe method for your situation.
Whitening Toothpastes; Facts and Fallacies
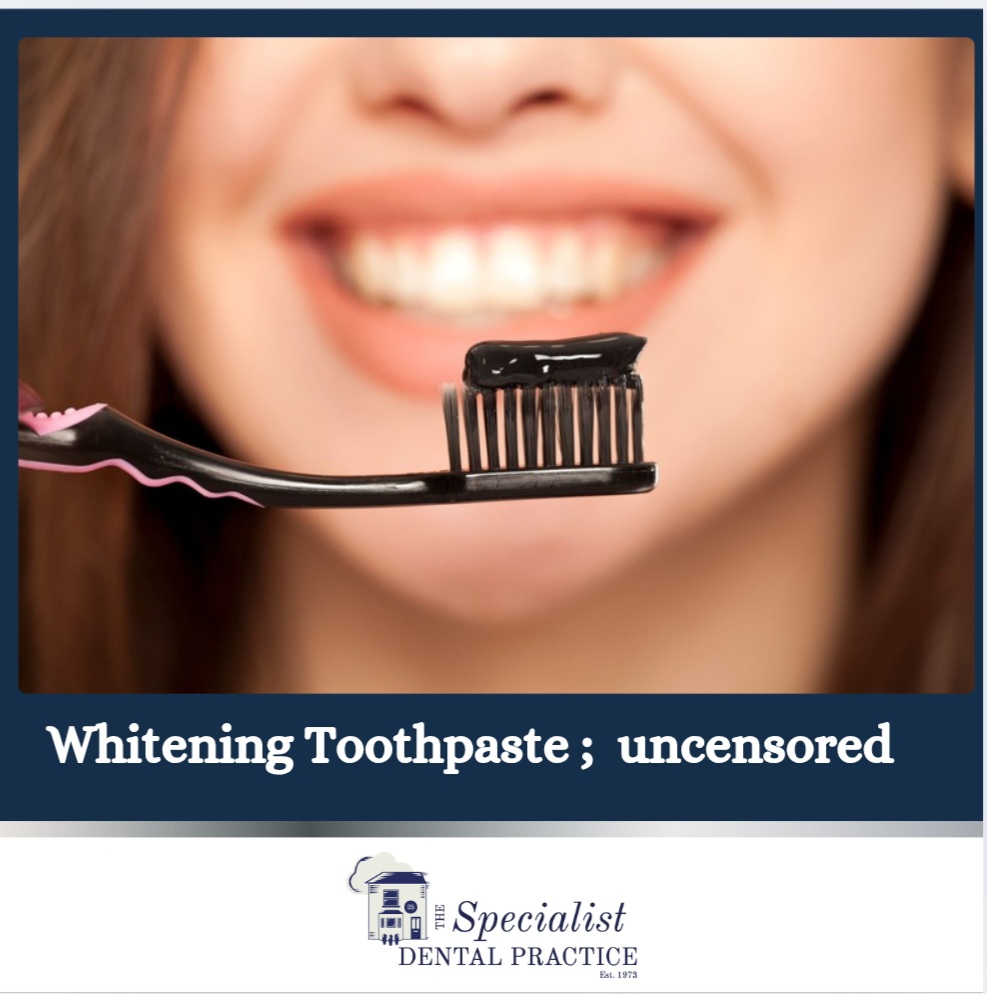
A Guide to Whitening Toothpastes in the UK: Efficacy Backed by Clinical Evidence
Whitening toothpastes are a popular choice for enhancing smiles, but how effective are they? In this blog, we’ll explore different types of whitening toothpastes available in the UK and evaluate their efficacy based on clinical evidence.
Abrasive-Based Whitening Toothpastes
These use mild abrasives like silica to remove surface stains caused by food, drinks, or smoking. While they can visibly improve brightness, clinical studies show they only remove extrinsic stains without altering the tooth’s natural color.
Efficacy: Effective for surface stain removal but not for deeper discoloration.
Enzyme-Based Whitening Toothpastes
Enzyme-based formulations (e.g., containing papain or bromelain) target protein pellicles that cause staining. Evidence suggests they can enhance stain removal without excessive abrasion, making them suitable for sensitive teeth.
Efficacy: Moderate improvement in surface brightness with minimal damage to enamel.
Peroxide-Based Whitening Toothpastes
Some toothpastes contain low levels of hydrogen or carbamide peroxide. Studies indicate they can help lighten intrinsic stains with consistent use over weeks. However, their whitening effect is less significant compared to professional bleaching.
Efficacy: Proven for mild intrinsic whitening, though results are subtle.
Charcoal Whitening Toothpastes
Charcoal-based products are widely marketed for whitening, but clinical evidence shows limited efficacy in removing stains. Excessive use may even harm enamel and gums due to high abrasiveness.
Efficacy: Poor stain removal with potential enamel damage.
Blue Covarine-Infused Toothpastes
These provide an immediate optical effect by depositing a blue pigment on teeth, creating the illusion of whiteness. While the results are temporary, studies support their effectiveness for a quick enhancement.
Efficacy: Temporary improvement in tooth brightness, ideal for short-term use.
Key Takeaways
Best for Surface Stains: Abrasive or enzyme-based toothpastes.
For Intrinsic Whitening: Peroxide-based formulas are most effective but offer mild results.
Quick Fix: Blue covarine toothpastes.
Avoid Overuse: Charcoal toothpastes due to abrasiveness.
For significant whitening or intrinsic stains, professional treatments remain the gold standard. Always consult your dentist to ensure the safest and most effective solution for your smile.
Dental Care and Coronavirus (COVID-19)
It is likely that the coronavirus will have an effect on your dental care.
Routine dental check-ups have been cancelled, and ongoing treatment plans may be disrupted. Where and how you access emergency dental treatment could also change.
This page includes advice on how you can access dental care, treatment and advice during the coronavirus pandemic.
Visiting the dental practice
If you are suffering with your oral health and need support, we are here to help.
To help stop the spread of coronavirus, we are advising against all routine and non-urgent dental treatment.
This includes:
Dental check-ups.
Preventive treatments such as scale and polish and fluoride varnishes.
Examinations and x-rays.
Appointments for braces.
Cosmetic dental treatment of any kind e.g. tooth whitening.
Routine denture treatment.
Treatments on teeth that are not painful e.g. fillings and extractions.
It is likely that your dental practice will contact you to postpone these appointments. If you do not hear from your dental practice, we recommend that you contact them to cancel your appointment and rearrange it for a later date.
In accordance to the instructions received by Public Health England (PHE) and CQC, all dental practices in England have temporarily ceased routine and non-urgent dental treatment. For emergency and urgent dental treatment, the dental surgery will provide remote (telephone or video-link) advice and assessment for further referral to the dedicated NHS Urgent Dental Care Centres (UDC) if necessary.
Whenever possible, stay at home and help stop the spread of coronavirus. This includes people of all ages – even if you do not have any symptoms or other health conditions.
Non-necessary dental treatment is not a reason for you to leave the home.
Urgent Dental Care
The NHS England has set up dedicated Urgent Dental Care Centres (UDC) for emergency and urgent dental conditions. Please note that this is not a walk-in service and requires appropriate referral by your dentist following remote triage.
If you are in pain, bleeding, swelling, or have had an accident and need urgent dental care, please contact your dental practice.
Please do not visit your dental practice without calling them first.
If you are not registered with any dental practice, please call 111 for further advice.
Dental Treatments in hospitals and A&E
To support NHS services and protect vital resources, it is important that you do not visit hospitals or A&E departments with dental problems.
If you need urgent or emergency dental treatment, contact your dental practice and they will be able to triage and direct you.
Dental care for vulnerable people and those with symptoms
If you need urgent dental care and are self-isolating because you have symptoms relating to coronavirus, or are a vulnerable person at higher risk, call NHS 111 or your dental practice.
The dental practice will be able to assess your needs and if necessary refer you to a special team/centre who will be able to treat you.
Buying oral health products
There is no shortage of oral health products like toothbrushes, toothpaste and mouthwash. Because of this, there is no need to stockpile them.
It is important to only buy what you need, when you need it.
Supermarkets remain open for essential food shopping and we advise that you buy any oral health products you need during this time. Please remember however to keep to social distancing rules and maintain two metres away from other shoppers.
When possible, instead of visiting supermarkets, we recommend that you buy oral health products online and have them delivered to your home.
Tips for good oral health
To help prevent dental problems from happening during coronavirus, here are some top tips for good oral health.
- Brush your teeth for two minutes, twice a day with a fluoride toothpaste.
- Do not share your toothbrushes. Keep the toothbrush clean and replace them frequently.
- The best time to brush is first thing in the morning and last thing at night before you go to bed.
- Cut down on how much sugar you have and how often you have it. This is even more important for children at home with increased temptation to snack and consume high sugar diet.
- Keep sugar consumption to mealtimes. This will reduce the time your teeth are under acid -attack.
- Maintain good hydration and avoid smoking and excessive consumption of alcohol.
- Use interdental brushes or floss to clean in between the teeth.
- Use non-alcohol based mouthwash daily to remove bad bacteria and keep fresh breath.
- Sugar-free chewing gum can help produce saliva and neutralise the plaque acids in your mouth.
More information and advice
Children coronavirus fact sheet, click here
For information about the coronavirus (COVID-19), please visit www.nhs.uk/conditions/coronavirus-covid-19/
The desire for the perfect Hollywood smile but at what cost?!

Cosmetic dentistry has become increasingly popular, largely as a result of social trends and increased media coverage. With the reality TV stars setting the trend in an industry now worth £2 billion, this understandable desire for the alleged ‘perfect smile’ needs to be tempered with an appropriate awareness of the significant risks associated with invasive cosmetic procedures such as veneers and crowns.
Patients need to be properly informed that elective removal of healthy enamel and dentine can result in pulpal injury and poorer periodontal health in the longer term, particularly if they are young. The duty of candour means that they ought to be informed that aggressive reduction of sound tooth tissue is not biologically neutral and results in structural weakening of their teeth. Less invasive procedures such as bleaching on its own or for example, combined with direct resin composite bonding, can satisfy many patient’s demands, while still being kinder to teeth and having much better fall-back positions for their future requirements.
It is the opinion of the British Endodontic Society, British Society for Restorative Dentistry, Restorative Dentistry UK, Dental Trauma UK, British Society of Prosthodontics and the British Society of Paediatric Dentistry that elective invasive cosmetic dental treatments can result in great benefit to patients, but that some aggressive treatments used to achieve them can produce significant morbidities in teeth which were previously healthy. This is a worrying and growing problem with many ethical, legal and biologic aspects, but many adverse outcomes for patients who request cosmetic dental improvements are preventable by using biologically safer initial approaches to treatment planning and its provision.
Dedicated personal, specialist care
The Specialist Dental Practice is the leading specialist restorative and implant dental practice in the county and has been setting the standards of specialist dentistry over the last 25 years.
The practice was established in 1973 and is conveniently located in the heart of Weybridge, Surrey. We are UK qualified and registered multi-specialist team offering specialist dental care of the highest quality and precision for the complex reconstruction cases involving dental implant therapy, gum disease treatment, root canal treatment, restoration of mutilated dentition and addressing challenges associated with partial and complete removable dentures.
We are delighted to welcome new referrals to our practice from both patients as well as professional colleagues.
Dental Implants
Essential questions to ask your dentist on dental implants
Taking the decision to have dental implants treatment is something most people will wish to consider quite carefully. Although this treatment can be an excellent long-term solution, it isn’t right for everybody and it is important to have a good understanding of exactly what is required. We have outlined a few essential questions and points you should be aware of before making your final decision.
WHAT ARE YOUR QUALIFICATIONS AND EXPERIENCE IN PLACING DENTAL IMPLANTS?
This is the most important question to ask and should be top of your list. Some clinicians have minimal training in placing dental implants and may only carry out this type of surgery a few times a year.
Our specialist care is based on dental specialties that are officially recognised by the General Dental Council UK. All accredited dental specialists are listed on the General Dental Council website www.gdc-uk.org. The specialist lists exist to:
• ensure high standards of training and assessment qualifying dentists to use a specialist title;
• indicate those dentists who possess recognised specialist knowledge, skills and attitudes;
• protect patients against unwarranted claims to be a specialist;
• facilitate appropriate referrals of patients;
• promote high standards of care by dentists qualified to use a specialist title; and
• encourage postgraduate education.
This list helps patients make an informed decision when they are looking for appropriately trained dentists to manage their dental care.
WHICH IMPLANT SYSTEMS DO YOU USE?
There are a few major dental implant companies that produce high-quality dental implants backed by years of research. These companies are well-known and well respected within the dental industry. There are numerous other companies that produce generic dental implants.
While these may still be of an acceptable quality, they lack the provenance of more widely known dental implant systems. There is another benefit of choosing dental implants made by one of the major companies as these implants are used worldwide. When you need an implant repaired or a component replaced or maintained, it is much easier to find a dentist willing to do this for you, no matter where you are in the world.
DO YOU PROVIDE COMPUTER GUIDED DENTAL IMPLANTS?
Computer guided dental implants surgery involves precisely planning using advanced diagnostics that include a cone beam CT scan and planning software. Once everything is planned, this computerised information is used to create a surgical guide or stent which allows precise placement of each implant.
We prefer to execute guided surgery where possible as it ensures your implant surgery is smoother, quicker and ultimately more comfortable and successful. Not all dentists will use this technique, but it is especially important when placing multiple implants where precision placement is even more vital.
Research shows that appropriately and precisely placed dental implants are less likely to have any problems and complications.
WILL IMPLANT SURGERY HURT?
You should not feel any pain during surgery based on effective local anaesthesia. We know many patients feel anxious at the thought of any oral surgery and if this applies to you then we can discuss additional sedation.
Our dental team is also very experienced at helping nervous patients feel at ease. Most of our patients will report no or very minimal discomfort that is very well managed with simple painkillers following implant surgery.
WILL I NEED A LONG TIME TO RECOVER AFTER IMPLANT SURGERY?
If you need just a single dental implant, you should be back to work the very next day. If you have multiple dental implants you might need a bit longer to recover; your dental implant dentist can give you more advice based on your situation.
Although you may feel some minor discomfort once the anaesthesia wears off, it is not uncommon to feel perfectly fine, especially after single dental implant placements. Again, this is something that can be discussed during your first consultation as it will depend on your treatment.
HOW LONG WILL IT TAKE TO COMPLETE IMPLANT TREATMENT?
Dental implant treatment can take up to several months to complete, as the surgery must be planned and once in place the implants need time to heal. It generally takes about 8-12 weeks for the dental implants to fully heal and to integrate with your jawbone, and the crown or bridge can be placed shortly after. Treatment may take slightly longer if you need bone grafts or tissue regeneration.
WILL I BE LEFT WITHOUT TEETH DURING IMPLANT HEALING?
This is a major concern for many people but there is no need to worry as temporary teeth can be provided while your implants heal. These temporary restorations can be fabricated before your implant surgery and may be placed immediately after surgery is completed.
WILL MY NEW IMPLANT TEETH LOOK NATURAL?
It is essential that your dental implants are placed in precisely the right position for the best functional and aesthetic effects. Here, at The Specialist dental Practice, our team are specialists in restoring and replacing missing teeth with crowns, bridges and dentures to the highest standards ensuring your new teeth are designed to look and feel wonderful. We also offer aftercare and advice on how to keep your implants clean.
HOW CAN I STOP MY DENTAL IMPLANTS FROM FAILING?
While some implants will fail naturally, a large part of implant success comes down to two factors:
• How well the implant is placed and the correct positioning in the jaw
• How well the implant is cared for after placement
Choosing a qualified and skilled implant dentist who is able to plan the correct positioning for your dental implants is key. Whilst you may think a general dentist is slightly cheaper, you may end up paying more in the future with implants that have not been placed correctly with significant potential complications.
The biggest misconception from dental implant patients is that once your dental implants are placed they will be there for life and are indestructible. The fact is, you will need to take care of your dental implants and make sure you regularly attend check-ups and clean your implants properly. Without this, your implants will have a larger chance of failing, both in a biologic and hardware sense.
SHOULD I GO ABROAD TO HAVE DENTAL IMPLANTS?
Dental tourism’ is a concept that has become increasingly popular over the last decade. Patients seek out dental treatment such as dental implants abroad and travel for the sole purpose of receiving cosmetic and restorative dentistry. The main attraction for patients is the cost of treatment in some other countries – it can look like prices are significantly cheaper, depending on the individual treatments. However, as with many things in life, what looks too good to be true often is. There are all kinds of hidden costs with choosing to get dental implants abroad including the prohibitive costs to fix a failing dental implant placed abroad, variation in the standard of care, and lack of long- term aftercare and maintenance plan.
Should you wish to seek more information on dental implant therapy, please contact the practice on 01932857585 or get in touch online info@weybridgedentist.co.uk to arrange for a consultation. In that way, we can assess for your individual needs and provide you with a customised treatment plan .
Specialist treatment for gum disease affecting teeth and dental implants

Understanding the importance of gum health
Gum disease affects many aspects of our life but is often overlooked as it has few symptoms in its early stages – that’s why it is often called ‘the silent disease’.
The vital thing about gum disease is that it is highly preventable and, especially in the early stages, quite easily treatable. Many studies link oral health to a number of significant conditions. There is strong evidence of the links between diabetes and gum disease. For Alzheimer’s and cardio health the role of gum disease is less clear. More than 45% of adults in the UK are affected by gum disease and, even at its most mild level, it can affect your quality of life.
Gum disease can affect dental implants as much as natural teeth. If you have any concerns about your dentition, speak to us and we will be happy to work with your dentist in managing your case.
Saving Your Natural Tooth
Specialist Endodontic Treatment
Nothing looks, feels or functions like your natural teeth, and endodontists are the experts in saving teeth. Keep smiling and eating the foods you love with endodontic treatment that can relieve your pain and save your teeth.
Sometimes your teeth may have infection or disease and will need additional care. When possible, you should always consider treatments to save your teeth. You may think, why not have a tooth pulled, especially if no one can see it, but you will know your tooth is missing and it will negatively impact your quality of life.
Don’t get a tooth pulled because you think its easier or more cost-effective. Missing teeth can cause other teeth to shift, affect your ability to properly chew and ruin your smile. Tooth extraction often is more painful than the infection itself, and replacing an extracted tooth with an artificial one requires additional dental visits that can quickly add up.
Modern endodontics offers advancements in technologies, procedures and materials, giving you many treatment options to save your natural teeth. It’s important to understand your choices and how they’ll impact both your tooth and your future dental health. It’s always best to retain your natural teeth whenever possible and endodontic treatment should be your first choice for the best health and cosmetic results. Endodontists are specialists in saving teeth. They can evaluate your condition and provide the best treatment plan to help you save your teeth for a lifetime.
Here are some tips for saving your teeth:
- When given a choice between tooth extraction and root canal treatment, always opt for a root canal. No denture, bridge or implant will look, feel and function as well as a natural tooth.
- Act immediately when you experience symptoms of swelling or pain. Most endodontists can accommodate emergency cases, even on weekends, ensuring you’ll be seen quickly.
- If your dentist recommends tooth extraction, ask whether the root canal is an option.If you’re told root canal is not an option, ask why and request a referral to an endodontist.
Root canal treatment from an endodontist is virtually painless and often leaves you with less discomfort during recovery than if you have your natural tooth extracted. Thanks to modern techniques and effective anesthesia, patients who experience root canals are six times more likely to describe it as painless than patients who have a tooth extracted! Take the time to learn more about root canal treatment and some of the common misconceptions about it and then take the first step to a pain-free, healthy mouth by visiting an endodontist.
How does endodontic treatment save the tooth?
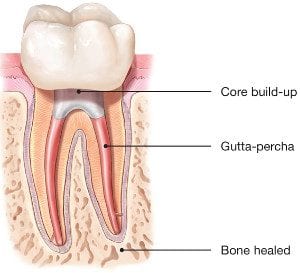
It’s necessary to have endodontic or root canal treatment when the inside of your tooth (the pulp) becomes inflamed or infected as a result of deep decay, repeated dental procedures, faulty crowns or a crack or chip in the tooth. Trauma to your tooth may also cause pulp damage even if the tooth has no visible chips or cracks. If pulp inflammation or infection is left untreated, it can cause pain or lead to an abscess.
When you undergo a root canal or other endodontic treatment, the inflamed or infected pulp is removed and the inside of the tooth is carefully cleaned and disinfected, then filled and sealed with a rubber-like material called gutta-percha. Afterward, the tooth is restored with a crown or filling for protection and will continue to function like any other tooth.
Endodontic treatment helps you maintain your natural smile, continue eating the foods you love and limits the need for ongoing dental work. With proper care, most teeth that have had root canal treatment can last a lifetime.
For more detailed information on root canal or to organise for a consultation, call us or get in touch online.
Biomimetic Dentistry
What is Biomimetic Dentistry?

Translated literally, biomimetic dentistry means to copy what is life-like. Nature has provided the most successful and ideal properties to our natural teeth. When restoring damaged, broken, and decayed teeth, the goal is to return the tooth to its original strength, function, and esthetics. Biomimetic dentistry accomplishes all of this in a conservative, strong, and attractive approach.
Why is it so important?
Tooth preservation and dental conservation lie at the heart of biomimetic dentistry.
Biomimetic dentistry replicates the strength, function, and aesthetics of natural teeth by replacing only damaged, decayed, and broken tooth structure. The principle employs techniques and materials that provide a perfect balance of nature, art and science.
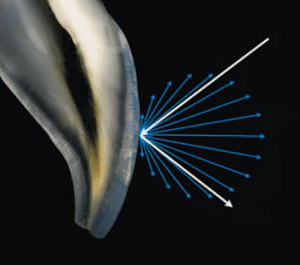
Teeth move, bend and have physical dynamics of force that must be accounted for while re-making the tooth with nature as our guide. Much of the amputation of tooth structure can be eliminated with modern science. We can say that tooth preservation and dental conservation lie at the heart of biomimetic dentistry.
The economic implications of not needing the advanced, invasive care seen in traditional (amputational) dentistry have profound positive effects on people’s lives. We can now help patients create healthy and happy mouths with simple, and often painless techniques!
Patients are happier and often spend less compared to conventional treatment.
Give us a call to find out more or book a consultation appointment.
Want to stop snoring?
As a condition that affects over 40% of the population, it is no surprise that the majority of us have been impacted by snoring in some way, shape or form. There are both varying degrees and varying types of snoring: it can be ‘simple’, or it can be symptomatic and may require further exploration. Regardless, there are a number of conditions associated, including:
- diminished energy
- lack of concentration
- increased risk of stress
- reduced libido
- high blood pressure
As well as the impact to the snorer, a lack of sleep on the bed partner’s behalf is also dangerous for their health and well-being. Many cases are reported by the bed-partner, with the snorer having very little awareness of their bedtime activities.

Thankfully, there are many interventions that can assist with snoring. Before discussing these, however, it is first important to highlight the cause.
What causes snoring?
Once we are asleep, our muscles relax. This can result in the soft tissues in the throat vibrating, causing the familiar snoring sound.
However, this doesn’t happen to everyone: there are a number of factors that can increase chances of snoring, including: obesity, gender, age, alcohol, and medication. For most sufferers, snoring occurs in isolation (simple snoring). In these cases, it is often the bed-partner that suffers, with the snorer unaware that they are causing such a disturbance. However, it can also take place as part of a more serious condition, obstructive sleep apnoea, which can be potentially life-threatening if not treated correctly.
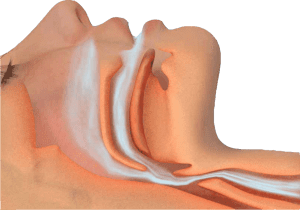
What is obstructive sleep apnoea (OSA)?
OSA is a serious condition where, for short periods of time, the airway becomes blocked during sleep, cutting off oxygen reaching the lungs. There are two types of breathing disruption associated with OSA:
- Apnoea – where the muscles collapse sufficiently enough to cause a total blockage of the airway for 10 seconds or more
- Hypopnoea – partial blockage of the airway that causes an airflow reduction of more than 50% for 10 seconds or more
Both of these problems can occur several times throughout the night and are most commonly recognised by loud snoring, paired with snorts, gasps, or laboured breathing. This leads to disruption for both the bed-partner AND the sufferer, with the snorer often waking feeling tired due to a night with reduced oxygen intake.
There are many associations with obstructive sleep apnoea, and, due to fat distribution, middle-aged males are twice as likely to suffer from OSA in comparison to middle-aged females. The discrepancy does start to level out, however, believed to be due to hormonal changes after menopause.
What are the treatments for snoring?
Though many snorers and tired bed-partners typically look to their doctor for help when it comes to snoring, their dentist arguably has a larger part to play – initially at least.
As snoring is typically caused by the lower jaw dropping back during sleep, the easiest way to stop it is to prevent the jaw from slipping backwards. This can be achieved with a device called a Mandibular Advancement Splint (MAS). Available from trained dentists, there are a number of devices available, one of which is the Sleepwell.

The most clinically proven MAS for the treatment of snoring & mild to moderate sleep apnoea, the Sleepwell is a two-piece device that is fully-adjustable by the wearer, and designed to hold your lower jaw forward. Holistically, however, there may be other behaviours that could assist with the problem, such as:
- Sleeping position – lying on your back inevitably is the worst position for snoring. Trying different positions may have a positive effect.
- Bed-time ‘hygiene’ – avoiding alcohol or caffeine in the evenings can help. Both muscle relaxants, they can increase the chances of snoring.
- Weight-loss – holding excess fat around your neck can play a major role in both snoring and sleep apnoea.
National Stop Snoring Week 23-27 April 2018
Cosmetic Dentistry- What You Should Know

Cosmetic dentistry has become increasingly popular, largely as a result of social trends and increased media coverage. This understandable desire for the alleged ‘perfect smile’ needs to be tempered with an appropriate awareness of the significant risks associated with invasive cosmetic procedures such as veneers and crowns. Patients need to be properly informed that elective removal of healthy enamel and dentine can result in pulpal injury and poorer periodontal health in the longer term, particularly if they are young. The duty of candour means that they ought to be informed that aggressive reduction of sound tooth tissue is not biologically neutral and results in structural weakening of their teeth. Less invasive procedures such as bleaching on its own or for example, combined with direct resin composite bonding, can satisfy many patient’s demands, while still being kinder to teeth and having much better fall-back positions for their future requirements. It is the opinion of the British Endodontic Society, British Society for Restorative Dentistry, Restorative Dentistry UK, Dental Trauma UK, British Society of Prosthodontics and the British Society of Paediatric Dentistry that elective invasive cosmetic dental treatments can result in great benefit to patients, but that some aggressive treatments used to achieve them can produce significant morbidities in teeth which were previously healthy. This is a worrying and growing problem with many ethical, legal and biologic aspects, but many adverse outcomes for patients who request cosmetic dental improvements are preventable by using biologically safer initial approaches to treatment planning and its provision.
Mouth Cancer Awareness Month

Most people have heard of cancer affecting parts of the body such as the lungs or breasts. However, cancer can also occur in the mouth, where the disease can affect the lips, tongue, cheeks and throat.
Anyone can be affected by mouth cancer, whether they have their own teeth or not. Mouth cancers are more common in people over 40, particularly men. However, research has shown that mouth cancer is becoming more common in younger patients and in women. In the last year more than 7,000 have been diagnosed with mouth cancer in the UK – an increase of more than a third compared to a decade ago.
Sadly, more than 1,800 people in the UK lose their life to mouth cancer every year. Many of these deaths could be prevented if the cancer was caught early enough. As it is, people with mouth cancer are more likely to die than those having cervical cancer or melanoma skin cancer.
Find out more at http://www.mouthcancer.org
Teeth whitening
Teeth whitening can be safe when done under the guidance of a dental professional or by following the instructions of over-the-counter products. However, it’s important to be aware of potential side effects, such as tooth sensitivity or gum irritation. Consult your dentist to discuss the best and safest whitening options for your specific needs.
Methods of teeth whitening:
**Professional Whitening:**This is done by a dentist and is the most effective method. It can involve in-office treatments using strong bleaching agents or custom-fitted trays with professional-grade whitening gels.
**Over-the-Counter (OTC) Products:** These include whitening toothpaste, strips, and gels. They are less potent than professional treatments and may take longer to show results.
Benefits of teeth whitening:
Improved Aesthetics: Whitening can remove stains and discoloration, enhancing the appearance of your teeth.
Boosted Confidence: A brighter smile often leads to increased self-confidence.
Non-Invasive: It’s a non-surgical and minimally invasive cosmetic dental procedure.
Risks and considerations:
Tooth Sensitivity: Whitening can cause temporary sensitivity to hot or cold foods and beverages.
Gum Irritation: Overuse or improper application of whitening products can irritate the gums.
Uneven Results: Whitening may not be equally effective on all teeth, leading to uneven results.
Duration of Effect: The duration of whitening effects varies; it may require touch-ups to maintain results.
Pre-existing Dental Issues: Whitening may not be suitable for everyone, especially those with dental restorations (crowns, fillings) as they do not respond to whitening treatments.
It’s crucial to consult with a dentist to discuss your specific needs and any potential risks associated with teeth whitening. They can help you choose the most appropriate and safe method for your situation.
Whitening Toothpastes; Facts and Fallacies
A Guide to Whitening Toothpastes in the UK: Efficacy Backed by Clinical Evidence
Whitening toothpastes are a popular choice for enhancing smiles, but how effective are they? In this blog, we’ll explore different types of whitening toothpastes available in the UK and evaluate their efficacy based on clinical evidence.
Abrasive-Based Whitening Toothpastes
These use mild abrasives like silica to remove surface stains caused by food, drinks, or smoking. While they can visibly improve brightness, clinical studies show they only remove extrinsic stains without altering the tooth’s natural color.
Efficacy: Effective for surface stain removal but not for deeper discoloration.
Enzyme-Based Whitening Toothpastes
Enzyme-based formulations (e.g., containing papain or bromelain) target protein pellicles that cause staining. Evidence suggests they can enhance stain removal without excessive abrasion, making them suitable for sensitive teeth.
Efficacy: Moderate improvement in surface brightness with minimal damage to enamel.
Peroxide-Based Whitening Toothpastes
Some toothpastes contain low levels of hydrogen or carbamide peroxide. Studies indicate they can help lighten intrinsic stains with consistent use over weeks. However, their whitening effect is less significant compared to professional bleaching.
Efficacy: Proven for mild intrinsic whitening, though results are subtle.
Charcoal Whitening Toothpastes
Charcoal-based products are widely marketed for whitening, but clinical evidence shows limited efficacy in removing stains. Excessive use may even harm enamel and gums due to high abrasiveness.
Efficacy: Poor stain removal with potential enamel damage.
Blue Covarine-Infused Toothpastes
These provide an immediate optical effect by depositing a blue pigment on teeth, creating the illusion of whiteness. While the results are temporary, studies support their effectiveness for a quick enhancement.
Efficacy: Temporary improvement in tooth brightness, ideal for short-term use.
Key Takeaways
Best for Surface Stains: Abrasive or enzyme-based toothpastes.
For Intrinsic Whitening: Peroxide-based formulas are most effective but offer mild results.
Quick Fix: Blue covarine toothpastes.
Avoid Overuse: Charcoal toothpastes due to abrasiveness.
For significant whitening or intrinsic stains, professional treatments remain the gold standard. Always consult your dentist to ensure the safest and most effective solution for your smile.
Dental Care and Coronavirus (COVID-19)
It is likely that the coronavirus will have an effect on your dental care.
Routine dental check-ups have been cancelled, and ongoing treatment plans may be disrupted. Where and how you access emergency dental treatment could also change.
This page includes advice on how you can access dental care, treatment and advice during the coronavirus pandemic.
Visiting the dental practice
If you are suffering with your oral health and need support, we are here to help.
To help stop the spread of coronavirus, we are advising against all routine and non-urgent dental treatment.
This includes:
Dental check-ups.
Preventive treatments such as scale and polish and fluoride varnishes.
Examinations and x-rays.
Appointments for braces.
Cosmetic dental treatment of any kind e.g. tooth whitening.
Routine denture treatment.
Treatments on teeth that are not painful e.g. fillings and extractions.
It is likely that your dental practice will contact you to postpone these appointments. If you do not hear from your dental practice, we recommend that you contact them to cancel your appointment and rearrange it for a later date.
In accordance to the instructions received by Public Health England (PHE) and CQC, all dental practices in England have temporarily ceased routine and non-urgent dental treatment. For emergency and urgent dental treatment, the dental surgery will provide remote (telephone or video-link) advice and assessment for further referral to the dedicated NHS Urgent Dental Care Centres (UDC) if necessary.
Whenever possible, stay at home and help stop the spread of coronavirus. This includes people of all ages – even if you do not have any symptoms or other health conditions.
Non-necessary dental treatment is not a reason for you to leave the home.
Urgent Dental Care
The NHS England has set up dedicated Urgent Dental Care Centres (UDC) for emergency and urgent dental conditions. Please note that this is not a walk-in service and requires appropriate referral by your dentist following remote triage.
If you are in pain, bleeding, swelling, or have had an accident and need urgent dental care, please contact your dental practice.
Please do not visit your dental practice without calling them first.
If you are not registered with any dental practice, please call 111 for further advice.
Dental Treatments in hospitals and A&E
To support NHS services and protect vital resources, it is important that you do not visit hospitals or A&E departments with dental problems.
If you need urgent or emergency dental treatment, contact your dental practice and they will be able to triage and direct you.
Dental care for vulnerable people and those with symptoms
If you need urgent dental care and are self-isolating because you have symptoms relating to coronavirus, or are a vulnerable person at higher risk, call NHS 111 or your dental practice.
The dental practice will be able to assess your needs and if necessary refer you to a special team/centre who will be able to treat you.
Buying oral health products
There is no shortage of oral health products like toothbrushes, toothpaste and mouthwash. Because of this, there is no need to stockpile them.
It is important to only buy what you need, when you need it.
Supermarkets remain open for essential food shopping and we advise that you buy any oral health products you need during this time. Please remember however to keep to social distancing rules and maintain two metres away from other shoppers.
When possible, instead of visiting supermarkets, we recommend that you buy oral health products online and have them delivered to your home.
Tips for good oral health
To help prevent dental problems from happening during coronavirus, here are some top tips for good oral health.
- Brush your teeth for two minutes, twice a day with a fluoride toothpaste.
- Do not share your toothbrushes. Keep the toothbrush clean and replace them frequently.
- The best time to brush is first thing in the morning and last thing at night before you go to bed.
- Cut down on how much sugar you have and how often you have it. This is even more important for children at home with increased temptation to snack and consume high sugar diet.
- Keep sugar consumption to mealtimes. This will reduce the time your teeth are under acid -attack.
- Maintain good hydration and avoid smoking and excessive consumption of alcohol.
- Use interdental brushes or floss to clean in between the teeth.
- Use non-alcohol based mouthwash daily to remove bad bacteria and keep fresh breath.
- Sugar-free chewing gum can help produce saliva and neutralise the plaque acids in your mouth.
More information and advice
Children coronavirus fact sheet, click here
For information about the coronavirus (COVID-19), please visit www.nhs.uk/conditions/coronavirus-covid-19/
The desire for the perfect Hollywood smile but at what cost?!

Cosmetic dentistry has become increasingly popular, largely as a result of social trends and increased media coverage. With the reality TV stars setting the trend in an industry now worth £2 billion, this understandable desire for the alleged ‘perfect smile’ needs to be tempered with an appropriate awareness of the significant risks associated with invasive cosmetic procedures such as veneers and crowns.
Patients need to be properly informed that elective removal of healthy enamel and dentine can result in pulpal injury and poorer periodontal health in the longer term, particularly if they are young. The duty of candour means that they ought to be informed that aggressive reduction of sound tooth tissue is not biologically neutral and results in structural weakening of their teeth. Less invasive procedures such as bleaching on its own or for example, combined with direct resin composite bonding, can satisfy many patient’s demands, while still being kinder to teeth and having much better fall-back positions for their future requirements.
It is the opinion of the British Endodontic Society, British Society for Restorative Dentistry, Restorative Dentistry UK, Dental Trauma UK, British Society of Prosthodontics and the British Society of Paediatric Dentistry that elective invasive cosmetic dental treatments can result in great benefit to patients, but that some aggressive treatments used to achieve them can produce significant morbidities in teeth which were previously healthy. This is a worrying and growing problem with many ethical, legal and biologic aspects, but many adverse outcomes for patients who request cosmetic dental improvements are preventable by using biologically safer initial approaches to treatment planning and its provision.
Dedicated personal, specialist care
The Specialist Dental Practice is the leading specialist restorative and implant dental practice in the county and has been setting the standards of specialist dentistry over the last 25 years.
The practice was established in 1973 and is conveniently located in the heart of Weybridge, Surrey. We are UK qualified and registered multi-specialist team offering specialist dental care of the highest quality and precision for the complex reconstruction cases involving dental implant therapy, gum disease treatment, root canal treatment, restoration of mutilated dentition and addressing challenges associated with partial and complete removable dentures.
We are delighted to welcome new referrals to our practice from both patients as well as professional colleagues.
Dental Implants
Essential questions to ask your dentist on dental implants
Taking the decision to have dental implants treatment is something most people will wish to consider quite carefully. Although this treatment can be an excellent long-term solution, it isn’t right for everybody and it is important to have a good understanding of exactly what is required. We have outlined a few essential questions and points you should be aware of before making your final decision.
WHAT ARE YOUR QUALIFICATIONS AND EXPERIENCE IN PLACING DENTAL IMPLANTS?
This is the most important question to ask and should be top of your list. Some clinicians have minimal training in placing dental implants and may only carry out this type of surgery a few times a year.
Our specialist care is based on dental specialties that are officially recognised by the General Dental Council UK. All accredited dental specialists are listed on the General Dental Council website www.gdc-uk.org. The specialist lists exist to:
• ensure high standards of training and assessment qualifying dentists to use a specialist title;
• indicate those dentists who possess recognised specialist knowledge, skills and attitudes;
• protect patients against unwarranted claims to be a specialist;
• facilitate appropriate referrals of patients;
• promote high standards of care by dentists qualified to use a specialist title; and
• encourage postgraduate education.
This list helps patients make an informed decision when they are looking for appropriately trained dentists to manage their dental care.
WHICH IMPLANT SYSTEMS DO YOU USE?
There are a few major dental implant companies that produce high-quality dental implants backed by years of research. These companies are well-known and well respected within the dental industry. There are numerous other companies that produce generic dental implants.
While these may still be of an acceptable quality, they lack the provenance of more widely known dental implant systems. There is another benefit of choosing dental implants made by one of the major companies as these implants are used worldwide. When you need an implant repaired or a component replaced or maintained, it is much easier to find a dentist willing to do this for you, no matter where you are in the world.
DO YOU PROVIDE COMPUTER GUIDED DENTAL IMPLANTS?
Computer guided dental implants surgery involves precisely planning using advanced diagnostics that include a cone beam CT scan and planning software. Once everything is planned, this computerised information is used to create a surgical guide or stent which allows precise placement of each implant.
We prefer to execute guided surgery where possible as it ensures your implant surgery is smoother, quicker and ultimately more comfortable and successful. Not all dentists will use this technique, but it is especially important when placing multiple implants where precision placement is even more vital.
Research shows that appropriately and precisely placed dental implants are less likely to have any problems and complications.
WILL IMPLANT SURGERY HURT?
You should not feel any pain during surgery based on effective local anaesthesia. We know many patients feel anxious at the thought of any oral surgery and if this applies to you then we can discuss additional sedation.
Our dental team is also very experienced at helping nervous patients feel at ease. Most of our patients will report no or very minimal discomfort that is very well managed with simple painkillers following implant surgery.
WILL I NEED A LONG TIME TO RECOVER AFTER IMPLANT SURGERY?
If you need just a single dental implant, you should be back to work the very next day. If you have multiple dental implants you might need a bit longer to recover; your dental implant dentist can give you more advice based on your situation.
Although you may feel some minor discomfort once the anaesthesia wears off, it is not uncommon to feel perfectly fine, especially after single dental implant placements. Again, this is something that can be discussed during your first consultation as it will depend on your treatment.
HOW LONG WILL IT TAKE TO COMPLETE IMPLANT TREATMENT?
Dental implant treatment can take up to several months to complete, as the surgery must be planned and once in place the implants need time to heal. It generally takes about 8-12 weeks for the dental implants to fully heal and to integrate with your jawbone, and the crown or bridge can be placed shortly after. Treatment may take slightly longer if you need bone grafts or tissue regeneration.
WILL I BE LEFT WITHOUT TEETH DURING IMPLANT HEALING?
This is a major concern for many people but there is no need to worry as temporary teeth can be provided while your implants heal. These temporary restorations can be fabricated before your implant surgery and may be placed immediately after surgery is completed.
WILL MY NEW IMPLANT TEETH LOOK NATURAL?
It is essential that your dental implants are placed in precisely the right position for the best functional and aesthetic effects. Here, at The Specialist dental Practice, our team are specialists in restoring and replacing missing teeth with crowns, bridges and dentures to the highest standards ensuring your new teeth are designed to look and feel wonderful. We also offer aftercare and advice on how to keep your implants clean.
HOW CAN I STOP MY DENTAL IMPLANTS FROM FAILING?
While some implants will fail naturally, a large part of implant success comes down to two factors:
• How well the implant is placed and the correct positioning in the jaw
• How well the implant is cared for after placement
Choosing a qualified and skilled implant dentist who is able to plan the correct positioning for your dental implants is key. Whilst you may think a general dentist is slightly cheaper, you may end up paying more in the future with implants that have not been placed correctly with significant potential complications.
The biggest misconception from dental implant patients is that once your dental implants are placed they will be there for life and are indestructible. The fact is, you will need to take care of your dental implants and make sure you regularly attend check-ups and clean your implants properly. Without this, your implants will have a larger chance of failing, both in a biologic and hardware sense.
SHOULD I GO ABROAD TO HAVE DENTAL IMPLANTS?
Dental tourism’ is a concept that has become increasingly popular over the last decade. Patients seek out dental treatment such as dental implants abroad and travel for the sole purpose of receiving cosmetic and restorative dentistry. The main attraction for patients is the cost of treatment in some other countries – it can look like prices are significantly cheaper, depending on the individual treatments. However, as with many things in life, what looks too good to be true often is. There are all kinds of hidden costs with choosing to get dental implants abroad including the prohibitive costs to fix a failing dental implant placed abroad, variation in the standard of care, and lack of long- term aftercare and maintenance plan.
Should you wish to seek more information on dental implant therapy, please contact the practice on 01932857585 or get in touch online info@weybridgedentist.co.uk to arrange for a consultation. In that way, we can assess for your individual needs and provide you with a customised treatment plan .
Specialist treatment for gum disease affecting teeth and dental implants

Understanding the importance of gum health
Gum disease affects many aspects of our life but is often overlooked as it has few symptoms in its early stages – that’s why it is often called ‘the silent disease’.
The vital thing about gum disease is that it is highly preventable and, especially in the early stages, quite easily treatable. Many studies link oral health to a number of significant conditions. There is strong evidence of the links between diabetes and gum disease. For Alzheimer’s and cardio health the role of gum disease is less clear. More than 45% of adults in the UK are affected by gum disease and, even at its most mild level, it can affect your quality of life.
Gum disease can affect dental implants as much as natural teeth. If you have any concerns about your dentition, speak to us and we will be happy to work with your dentist in managing your case.
Saving Your Natural Tooth
Specialist Endodontic Treatment
Nothing looks, feels or functions like your natural teeth, and endodontists are the experts in saving teeth. Keep smiling and eating the foods you love with endodontic treatment that can relieve your pain and save your teeth.
Sometimes your teeth may have infection or disease and will need additional care. When possible, you should always consider treatments to save your teeth. You may think, why not have a tooth pulled, especially if no one can see it, but you will know your tooth is missing and it will negatively impact your quality of life.
Don’t get a tooth pulled because you think its easier or more cost-effective. Missing teeth can cause other teeth to shift, affect your ability to properly chew and ruin your smile. Tooth extraction often is more painful than the infection itself, and replacing an extracted tooth with an artificial one requires additional dental visits that can quickly add up.
Modern endodontics offers advancements in technologies, procedures and materials, giving you many treatment options to save your natural teeth. It’s important to understand your choices and how they’ll impact both your tooth and your future dental health. It’s always best to retain your natural teeth whenever possible and endodontic treatment should be your first choice for the best health and cosmetic results. Endodontists are specialists in saving teeth. They can evaluate your condition and provide the best treatment plan to help you save your teeth for a lifetime.
Here are some tips for saving your teeth:
- When given a choice between tooth extraction and root canal treatment, always opt for a root canal. No denture, bridge or implant will look, feel and function as well as a natural tooth.
- Act immediately when you experience symptoms of swelling or pain. Most endodontists can accommodate emergency cases, even on weekends, ensuring you’ll be seen quickly.
- If your dentist recommends tooth extraction, ask whether the root canal is an option.If you’re told root canal is not an option, ask why and request a referral to an endodontist.
Root canal treatment from an endodontist is virtually painless and often leaves you with less discomfort during recovery than if you have your natural tooth extracted. Thanks to modern techniques and effective anesthesia, patients who experience root canals are six times more likely to describe it as painless than patients who have a tooth extracted! Take the time to learn more about root canal treatment and some of the common misconceptions about it and then take the first step to a pain-free, healthy mouth by visiting an endodontist.
How does endodontic treatment save the tooth?
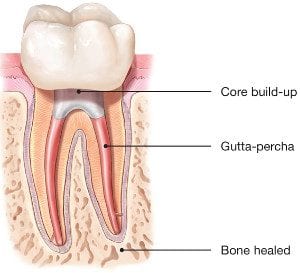
It’s necessary to have endodontic or root canal treatment when the inside of your tooth (the pulp) becomes inflamed or infected as a result of deep decay, repeated dental procedures, faulty crowns or a crack or chip in the tooth. Trauma to your tooth may also cause pulp damage even if the tooth has no visible chips or cracks. If pulp inflammation or infection is left untreated, it can cause pain or lead to an abscess.
When you undergo a root canal or other endodontic treatment, the inflamed or infected pulp is removed and the inside of the tooth is carefully cleaned and disinfected, then filled and sealed with a rubber-like material called gutta-percha. Afterward, the tooth is restored with a crown or filling for protection and will continue to function like any other tooth.
Endodontic treatment helps you maintain your natural smile, continue eating the foods you love and limits the need for ongoing dental work. With proper care, most teeth that have had root canal treatment can last a lifetime.
For more detailed information on root canal or to organise for a consultation, call us or get in touch online.
Biomimetic Dentistry
What is Biomimetic Dentistry?

Translated literally, biomimetic dentistry means to copy what is life-like. Nature has provided the most successful and ideal properties to our natural teeth. When restoring damaged, broken, and decayed teeth, the goal is to return the tooth to its original strength, function, and esthetics. Biomimetic dentistry accomplishes all of this in a conservative, strong, and attractive approach.
Why is it so important?
Tooth preservation and dental conservation lie at the heart of biomimetic dentistry.
Biomimetic dentistry replicates the strength, function, and aesthetics of natural teeth by replacing only damaged, decayed, and broken tooth structure. The principle employs techniques and materials that provide a perfect balance of nature, art and science.
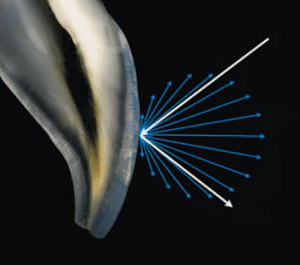
Teeth move, bend and have physical dynamics of force that must be accounted for while re-making the tooth with nature as our guide. Much of the amputation of tooth structure can be eliminated with modern science. We can say that tooth preservation and dental conservation lie at the heart of biomimetic dentistry.
The economic implications of not needing the advanced, invasive care seen in traditional (amputational) dentistry have profound positive effects on people’s lives. We can now help patients create healthy and happy mouths with simple, and often painless techniques!
Patients are happier and often spend less compared to conventional treatment.
Give us a call to find out more or book a consultation appointment.
Want to stop snoring?
As a condition that affects over 40% of the population, it is no surprise that the majority of us have been impacted by snoring in some way, shape or form. There are both varying degrees and varying types of snoring: it can be ‘simple’, or it can be symptomatic and may require further exploration. Regardless, there are a number of conditions associated, including:
- diminished energy
- lack of concentration
- increased risk of stress
- reduced libido
- high blood pressure
As well as the impact to the snorer, a lack of sleep on the bed partner’s behalf is also dangerous for their health and well-being. Many cases are reported by the bed-partner, with the snorer having very little awareness of their bedtime activities.

Thankfully, there are many interventions that can assist with snoring. Before discussing these, however, it is first important to highlight the cause.
What causes snoring?
Once we are asleep, our muscles relax. This can result in the soft tissues in the throat vibrating, causing the familiar snoring sound.
However, this doesn’t happen to everyone: there are a number of factors that can increase chances of snoring, including: obesity, gender, age, alcohol, and medication. For most sufferers, snoring occurs in isolation (simple snoring). In these cases, it is often the bed-partner that suffers, with the snorer unaware that they are causing such a disturbance. However, it can also take place as part of a more serious condition, obstructive sleep apnoea, which can be potentially life-threatening if not treated correctly.
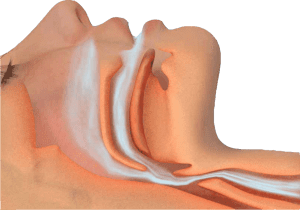
What is obstructive sleep apnoea (OSA)?
OSA is a serious condition where, for short periods of time, the airway becomes blocked during sleep, cutting off oxygen reaching the lungs. There are two types of breathing disruption associated with OSA:
- Apnoea – where the muscles collapse sufficiently enough to cause a total blockage of the airway for 10 seconds or more
- Hypopnoea – partial blockage of the airway that causes an airflow reduction of more than 50% for 10 seconds or more
Both of these problems can occur several times throughout the night and are most commonly recognised by loud snoring, paired with snorts, gasps, or laboured breathing. This leads to disruption for both the bed-partner AND the sufferer, with the snorer often waking feeling tired due to a night with reduced oxygen intake.
There are many associations with obstructive sleep apnoea, and, due to fat distribution, middle-aged males are twice as likely to suffer from OSA in comparison to middle-aged females. The discrepancy does start to level out, however, believed to be due to hormonal changes after menopause.
What are the treatments for snoring?
Though many snorers and tired bed-partners typically look to their doctor for help when it comes to snoring, their dentist arguably has a larger part to play – initially at least.
As snoring is typically caused by the lower jaw dropping back during sleep, the easiest way to stop it is to prevent the jaw from slipping backwards. This can be achieved with a device called a Mandibular Advancement Splint (MAS). Available from trained dentists, there are a number of devices available, one of which is the Sleepwell.

The most clinically proven MAS for the treatment of snoring & mild to moderate sleep apnoea, the Sleepwell is a two-piece device that is fully-adjustable by the wearer, and designed to hold your lower jaw forward. Holistically, however, there may be other behaviours that could assist with the problem, such as:
- Sleeping position – lying on your back inevitably is the worst position for snoring. Trying different positions may have a positive effect.
- Bed-time ‘hygiene’ – avoiding alcohol or caffeine in the evenings can help. Both muscle relaxants, they can increase the chances of snoring.
- Weight-loss – holding excess fat around your neck can play a major role in both snoring and sleep apnoea.
National Stop Snoring Week 23-27 April 2018
Cosmetic Dentistry- What You Should Know

Cosmetic dentistry has become increasingly popular, largely as a result of social trends and increased media coverage. This understandable desire for the alleged ‘perfect smile’ needs to be tempered with an appropriate awareness of the significant risks associated with invasive cosmetic procedures such as veneers and crowns. Patients need to be properly informed that elective removal of healthy enamel and dentine can result in pulpal injury and poorer periodontal health in the longer term, particularly if they are young. The duty of candour means that they ought to be informed that aggressive reduction of sound tooth tissue is not biologically neutral and results in structural weakening of their teeth. Less invasive procedures such as bleaching on its own or for example, combined with direct resin composite bonding, can satisfy many patient’s demands, while still being kinder to teeth and having much better fall-back positions for their future requirements. It is the opinion of the British Endodontic Society, British Society for Restorative Dentistry, Restorative Dentistry UK, Dental Trauma UK, British Society of Prosthodontics and the British Society of Paediatric Dentistry that elective invasive cosmetic dental treatments can result in great benefit to patients, but that some aggressive treatments used to achieve them can produce significant morbidities in teeth which were previously healthy. This is a worrying and growing problem with many ethical, legal and biologic aspects, but many adverse outcomes for patients who request cosmetic dental improvements are preventable by using biologically safer initial approaches to treatment planning and its provision.
Mouth Cancer Awareness Month

Most people have heard of cancer affecting parts of the body such as the lungs or breasts. However, cancer can also occur in the mouth, where the disease can affect the lips, tongue, cheeks and throat.
Anyone can be affected by mouth cancer, whether they have their own teeth or not. Mouth cancers are more common in people over 40, particularly men. However, research has shown that mouth cancer is becoming more common in younger patients and in women. In the last year more than 7,000 have been diagnosed with mouth cancer in the UK – an increase of more than a third compared to a decade ago.
Sadly, more than 1,800 people in the UK lose their life to mouth cancer every year. Many of these deaths could be prevented if the cancer was caught early enough. As it is, people with mouth cancer are more likely to die than those having cervical cancer or melanoma skin cancer.
Find out more at http://www.mouthcancer.org
Teeth whitening
Teeth whitening can be safe when done under the guidance of a dental professional or by following the instructions of over-the-counter products. However, it’s important to be aware of potential side effects, such as tooth sensitivity or gum irritation. Consult your dentist to discuss the best and safest whitening options for your specific needs.
Methods of teeth whitening:
**Professional Whitening:**This is done by a dentist and is the most effective method. It can involve in-office treatments using strong bleaching agents or custom-fitted trays with professional-grade whitening gels.
**Over-the-Counter (OTC) Products:** These include whitening toothpaste, strips, and gels. They are less potent than professional treatments and may take longer to show results.
Benefits of teeth whitening:
Improved Aesthetics: Whitening can remove stains and discoloration, enhancing the appearance of your teeth.
Boosted Confidence: A brighter smile often leads to increased self-confidence.
Non-Invasive: It’s a non-surgical and minimally invasive cosmetic dental procedure.
Risks and considerations:
Tooth Sensitivity: Whitening can cause temporary sensitivity to hot or cold foods and beverages.
Gum Irritation: Overuse or improper application of whitening products can irritate the gums.
Uneven Results: Whitening may not be equally effective on all teeth, leading to uneven results.
Duration of Effect: The duration of whitening effects varies; it may require touch-ups to maintain results.
Pre-existing Dental Issues: Whitening may not be suitable for everyone, especially those with dental restorations (crowns, fillings) as they do not respond to whitening treatments.
It’s crucial to consult with a dentist to discuss your specific needs and any potential risks associated with teeth whitening. They can help you choose the most appropriate and safe method for your situation.
Whitening Toothpastes; Facts and Fallacies
A Guide to Whitening Toothpastes in the UK: Efficacy Backed by Clinical Evidence
Whitening toothpastes are a popular choice for enhancing smiles, but how effective are they? In this blog, we’ll explore different types of whitening toothpastes available in the UK and evaluate their efficacy based on clinical evidence.
Abrasive-Based Whitening Toothpastes
These use mild abrasives like silica to remove surface stains caused by food, drinks, or smoking. While they can visibly improve brightness, clinical studies show they only remove extrinsic stains without altering the tooth’s natural color.
Efficacy: Effective for surface stain removal but not for deeper discoloration.
Enzyme-Based Whitening Toothpastes
Enzyme-based formulations (e.g., containing papain or bromelain) target protein pellicles that cause staining. Evidence suggests they can enhance stain removal without excessive abrasion, making them suitable for sensitive teeth.
Efficacy: Moderate improvement in surface brightness with minimal damage to enamel.
Peroxide-Based Whitening Toothpastes
Some toothpastes contain low levels of hydrogen or carbamide peroxide. Studies indicate they can help lighten intrinsic stains with consistent use over weeks. However, their whitening effect is less significant compared to professional bleaching.
Efficacy: Proven for mild intrinsic whitening, though results are subtle.
Charcoal Whitening Toothpastes
Charcoal-based products are widely marketed for whitening, but clinical evidence shows limited efficacy in removing stains. Excessive use may even harm enamel and gums due to high abrasiveness.
Efficacy: Poor stain removal with potential enamel damage.
Blue Covarine-Infused Toothpastes
These provide an immediate optical effect by depositing a blue pigment on teeth, creating the illusion of whiteness. While the results are temporary, studies support their effectiveness for a quick enhancement.
Efficacy: Temporary improvement in tooth brightness, ideal for short-term use.
Key Takeaways
Best for Surface Stains: Abrasive or enzyme-based toothpastes.
For Intrinsic Whitening: Peroxide-based formulas are most effective but offer mild results.
Quick Fix: Blue covarine toothpastes.
Avoid Overuse: Charcoal toothpastes due to abrasiveness.
For significant whitening or intrinsic stains, professional treatments remain the gold standard. Always consult your dentist to ensure the safest and most effective solution for your smile.
Dental Care and Coronavirus (COVID-19)
It is likely that the coronavirus will have an effect on your dental care.
Routine dental check-ups have been cancelled, and ongoing treatment plans may be disrupted. Where and how you access emergency dental treatment could also change.
This page includes advice on how you can access dental care, treatment and advice during the coronavirus pandemic.
Visiting the dental practice
If you are suffering with your oral health and need support, we are here to help.
To help stop the spread of coronavirus, we are advising against all routine and non-urgent dental treatment.
This includes:
Dental check-ups.
Preventive treatments such as scale and polish and fluoride varnishes.
Examinations and x-rays.
Appointments for braces.
Cosmetic dental treatment of any kind e.g. tooth whitening.
Routine denture treatment.
Treatments on teeth that are not painful e.g. fillings and extractions.
It is likely that your dental practice will contact you to postpone these appointments. If you do not hear from your dental practice, we recommend that you contact them to cancel your appointment and rearrange it for a later date.
In accordance to the instructions received by Public Health England (PHE) and CQC, all dental practices in England have temporarily ceased routine and non-urgent dental treatment. For emergency and urgent dental treatment, the dental surgery will provide remote (telephone or video-link) advice and assessment for further referral to the dedicated NHS Urgent Dental Care Centres (UDC) if necessary.
Whenever possible, stay at home and help stop the spread of coronavirus. This includes people of all ages – even if you do not have any symptoms or other health conditions.
Non-necessary dental treatment is not a reason for you to leave the home.
Urgent Dental Care
The NHS England has set up dedicated Urgent Dental Care Centres (UDC) for emergency and urgent dental conditions. Please note that this is not a walk-in service and requires appropriate referral by your dentist following remote triage.
If you are in pain, bleeding, swelling, or have had an accident and need urgent dental care, please contact your dental practice.
Please do not visit your dental practice without calling them first.
If you are not registered with any dental practice, please call 111 for further advice.
Dental Treatments in hospitals and A&E
To support NHS services and protect vital resources, it is important that you do not visit hospitals or A&E departments with dental problems.
If you need urgent or emergency dental treatment, contact your dental practice and they will be able to triage and direct you.
Dental care for vulnerable people and those with symptoms
If you need urgent dental care and are self-isolating because you have symptoms relating to coronavirus, or are a vulnerable person at higher risk, call NHS 111 or your dental practice.
The dental practice will be able to assess your needs and if necessary refer you to a special team/centre who will be able to treat you.
Buying oral health products
There is no shortage of oral health products like toothbrushes, toothpaste and mouthwash. Because of this, there is no need to stockpile them.
It is important to only buy what you need, when you need it.
Supermarkets remain open for essential food shopping and we advise that you buy any oral health products you need during this time. Please remember however to keep to social distancing rules and maintain two metres away from other shoppers.
When possible, instead of visiting supermarkets, we recommend that you buy oral health products online and have them delivered to your home.
Tips for good oral health
To help prevent dental problems from happening during coronavirus, here are some top tips for good oral health.
- Brush your teeth for two minutes, twice a day with a fluoride toothpaste.
- Do not share your toothbrushes. Keep the toothbrush clean and replace them frequently.
- The best time to brush is first thing in the morning and last thing at night before you go to bed.
- Cut down on how much sugar you have and how often you have it. This is even more important for children at home with increased temptation to snack and consume high sugar diet.
- Keep sugar consumption to mealtimes. This will reduce the time your teeth are under acid -attack.
- Maintain good hydration and avoid smoking and excessive consumption of alcohol.
- Use interdental brushes or floss to clean in between the teeth.
- Use non-alcohol based mouthwash daily to remove bad bacteria and keep fresh breath.
- Sugar-free chewing gum can help produce saliva and neutralise the plaque acids in your mouth.
More information and advice
Children coronavirus fact sheet, click here
For information about the coronavirus (COVID-19), please visit www.nhs.uk/conditions/coronavirus-covid-19/
The desire for the perfect Hollywood smile but at what cost?!

Cosmetic dentistry has become increasingly popular, largely as a result of social trends and increased media coverage. With the reality TV stars setting the trend in an industry now worth £2 billion, this understandable desire for the alleged ‘perfect smile’ needs to be tempered with an appropriate awareness of the significant risks associated with invasive cosmetic procedures such as veneers and crowns.
Patients need to be properly informed that elective removal of healthy enamel and dentine can result in pulpal injury and poorer periodontal health in the longer term, particularly if they are young. The duty of candour means that they ought to be informed that aggressive reduction of sound tooth tissue is not biologically neutral and results in structural weakening of their teeth. Less invasive procedures such as bleaching on its own or for example, combined with direct resin composite bonding, can satisfy many patient’s demands, while still being kinder to teeth and having much better fall-back positions for their future requirements.
It is the opinion of the British Endodontic Society, British Society for Restorative Dentistry, Restorative Dentistry UK, Dental Trauma UK, British Society of Prosthodontics and the British Society of Paediatric Dentistry that elective invasive cosmetic dental treatments can result in great benefit to patients, but that some aggressive treatments used to achieve them can produce significant morbidities in teeth which were previously healthy. This is a worrying and growing problem with many ethical, legal and biologic aspects, but many adverse outcomes for patients who request cosmetic dental improvements are preventable by using biologically safer initial approaches to treatment planning and its provision.
Dedicated personal, specialist care
The Specialist Dental Practice is the leading specialist restorative and implant dental practice in the county and has been setting the standards of specialist dentistry over the last 25 years.
The practice was established in 1973 and is conveniently located in the heart of Weybridge, Surrey. We are UK qualified and registered multi-specialist team offering specialist dental care of the highest quality and precision for the complex reconstruction cases involving dental implant therapy, gum disease treatment, root canal treatment, restoration of mutilated dentition and addressing challenges associated with partial and complete removable dentures.
We are delighted to welcome new referrals to our practice from both patients as well as professional colleagues.
Dental Implants
Essential questions to ask your dentist on dental implants
Taking the decision to have dental implants treatment is something most people will wish to consider quite carefully. Although this treatment can be an excellent long-term solution, it isn’t right for everybody and it is important to have a good understanding of exactly what is required. We have outlined a few essential questions and points you should be aware of before making your final decision.
WHAT ARE YOUR QUALIFICATIONS AND EXPERIENCE IN PLACING DENTAL IMPLANTS?
This is the most important question to ask and should be top of your list. Some clinicians have minimal training in placing dental implants and may only carry out this type of surgery a few times a year.
Our specialist care is based on dental specialties that are officially recognised by the General Dental Council UK. All accredited dental specialists are listed on the General Dental Council website www.gdc-uk.org. The specialist lists exist to:
• ensure high standards of training and assessment qualifying dentists to use a specialist title;
• indicate those dentists who possess recognised specialist knowledge, skills and attitudes;
• protect patients against unwarranted claims to be a specialist;
• facilitate appropriate referrals of patients;
• promote high standards of care by dentists qualified to use a specialist title; and
• encourage postgraduate education.
This list helps patients make an informed decision when they are looking for appropriately trained dentists to manage their dental care.
WHICH IMPLANT SYSTEMS DO YOU USE?
There are a few major dental implant companies that produce high-quality dental implants backed by years of research. These companies are well-known and well respected within the dental industry. There are numerous other companies that produce generic dental implants.
While these may still be of an acceptable quality, they lack the provenance of more widely known dental implant systems. There is another benefit of choosing dental implants made by one of the major companies as these implants are used worldwide. When you need an implant repaired or a component replaced or maintained, it is much easier to find a dentist willing to do this for you, no matter where you are in the world.
DO YOU PROVIDE COMPUTER GUIDED DENTAL IMPLANTS?
Computer guided dental implants surgery involves precisely planning using advanced diagnostics that include a cone beam CT scan and planning software. Once everything is planned, this computerised information is used to create a surgical guide or stent which allows precise placement of each implant.
We prefer to execute guided surgery where possible as it ensures your implant surgery is smoother, quicker and ultimately more comfortable and successful. Not all dentists will use this technique, but it is especially important when placing multiple implants where precision placement is even more vital.
Research shows that appropriately and precisely placed dental implants are less likely to have any problems and complications.
WILL IMPLANT SURGERY HURT?
You should not feel any pain during surgery based on effective local anaesthesia. We know many patients feel anxious at the thought of any oral surgery and if this applies to you then we can discuss additional sedation.
Our dental team is also very experienced at helping nervous patients feel at ease. Most of our patients will report no or very minimal discomfort that is very well managed with simple painkillers following implant surgery.
WILL I NEED A LONG TIME TO RECOVER AFTER IMPLANT SURGERY?
If you need just a single dental implant, you should be back to work the very next day. If you have multiple dental implants you might need a bit longer to recover; your dental implant dentist can give you more advice based on your situation.
Although you may feel some minor discomfort once the anaesthesia wears off, it is not uncommon to feel perfectly fine, especially after single dental implant placements. Again, this is something that can be discussed during your first consultation as it will depend on your treatment.
HOW LONG WILL IT TAKE TO COMPLETE IMPLANT TREATMENT?
Dental implant treatment can take up to several months to complete, as the surgery must be planned and once in place the implants need time to heal. It generally takes about 8-12 weeks for the dental implants to fully heal and to integrate with your jawbone, and the crown or bridge can be placed shortly after. Treatment may take slightly longer if you need bone grafts or tissue regeneration.
WILL I BE LEFT WITHOUT TEETH DURING IMPLANT HEALING?
This is a major concern for many people but there is no need to worry as temporary teeth can be provided while your implants heal. These temporary restorations can be fabricated before your implant surgery and may be placed immediately after surgery is completed.
WILL MY NEW IMPLANT TEETH LOOK NATURAL?
It is essential that your dental implants are placed in precisely the right position for the best functional and aesthetic effects. Here, at The Specialist dental Practice, our team are specialists in restoring and replacing missing teeth with crowns, bridges and dentures to the highest standards ensuring your new teeth are designed to look and feel wonderful. We also offer aftercare and advice on how to keep your implants clean.
HOW CAN I STOP MY DENTAL IMPLANTS FROM FAILING?
While some implants will fail naturally, a large part of implant success comes down to two factors:
• How well the implant is placed and the correct positioning in the jaw
• How well the implant is cared for after placement
Choosing a qualified and skilled implant dentist who is able to plan the correct positioning for your dental implants is key. Whilst you may think a general dentist is slightly cheaper, you may end up paying more in the future with implants that have not been placed correctly with significant potential complications.
The biggest misconception from dental implant patients is that once your dental implants are placed they will be there for life and are indestructible. The fact is, you will need to take care of your dental implants and make sure you regularly attend check-ups and clean your implants properly. Without this, your implants will have a larger chance of failing, both in a biologic and hardware sense.
SHOULD I GO ABROAD TO HAVE DENTAL IMPLANTS?
Dental tourism’ is a concept that has become increasingly popular over the last decade. Patients seek out dental treatment such as dental implants abroad and travel for the sole purpose of receiving cosmetic and restorative dentistry. The main attraction for patients is the cost of treatment in some other countries – it can look like prices are significantly cheaper, depending on the individual treatments. However, as with many things in life, what looks too good to be true often is. There are all kinds of hidden costs with choosing to get dental implants abroad including the prohibitive costs to fix a failing dental implant placed abroad, variation in the standard of care, and lack of long- term aftercare and maintenance plan.
Should you wish to seek more information on dental implant therapy, please contact the practice on 01932857585 or get in touch online info@weybridgedentist.co.uk to arrange for a consultation. In that way, we can assess for your individual needs and provide you with a customised treatment plan .
Specialist treatment for gum disease affecting teeth and dental implants

Understanding the importance of gum health
Gum disease affects many aspects of our life but is often overlooked as it has few symptoms in its early stages – that’s why it is often called ‘the silent disease’.
The vital thing about gum disease is that it is highly preventable and, especially in the early stages, quite easily treatable. Many studies link oral health to a number of significant conditions. There is strong evidence of the links between diabetes and gum disease. For Alzheimer’s and cardio health the role of gum disease is less clear. More than 45% of adults in the UK are affected by gum disease and, even at its most mild level, it can affect your quality of life.
Gum disease can affect dental implants as much as natural teeth. If you have any concerns about your dentition, speak to us and we will be happy to work with your dentist in managing your case.
Saving Your Natural Tooth
Specialist Endodontic Treatment
Nothing looks, feels or functions like your natural teeth, and endodontists are the experts in saving teeth. Keep smiling and eating the foods you love with endodontic treatment that can relieve your pain and save your teeth.
Sometimes your teeth may have infection or disease and will need additional care. When possible, you should always consider treatments to save your teeth. You may think, why not have a tooth pulled, especially if no one can see it, but you will know your tooth is missing and it will negatively impact your quality of life.
Don’t get a tooth pulled because you think its easier or more cost-effective. Missing teeth can cause other teeth to shift, affect your ability to properly chew and ruin your smile. Tooth extraction often is more painful than the infection itself, and replacing an extracted tooth with an artificial one requires additional dental visits that can quickly add up.
Modern endodontics offers advancements in technologies, procedures and materials, giving you many treatment options to save your natural teeth. It’s important to understand your choices and how they’ll impact both your tooth and your future dental health. It’s always best to retain your natural teeth whenever possible and endodontic treatment should be your first choice for the best health and cosmetic results. Endodontists are specialists in saving teeth. They can evaluate your condition and provide the best treatment plan to help you save your teeth for a lifetime.
Here are some tips for saving your teeth:
- When given a choice between tooth extraction and root canal treatment, always opt for a root canal. No denture, bridge or implant will look, feel and function as well as a natural tooth.
- Act immediately when you experience symptoms of swelling or pain. Most endodontists can accommodate emergency cases, even on weekends, ensuring you’ll be seen quickly.
- If your dentist recommends tooth extraction, ask whether the root canal is an option.If you’re told root canal is not an option, ask why and request a referral to an endodontist.
Root canal treatment from an endodontist is virtually painless and often leaves you with less discomfort during recovery than if you have your natural tooth extracted. Thanks to modern techniques and effective anesthesia, patients who experience root canals are six times more likely to describe it as painless than patients who have a tooth extracted! Take the time to learn more about root canal treatment and some of the common misconceptions about it and then take the first step to a pain-free, healthy mouth by visiting an endodontist.
How does endodontic treatment save the tooth?
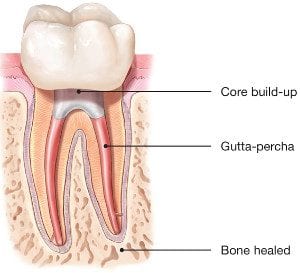
It’s necessary to have endodontic or root canal treatment when the inside of your tooth (the pulp) becomes inflamed or infected as a result of deep decay, repeated dental procedures, faulty crowns or a crack or chip in the tooth. Trauma to your tooth may also cause pulp damage even if the tooth has no visible chips or cracks. If pulp inflammation or infection is left untreated, it can cause pain or lead to an abscess.
When you undergo a root canal or other endodontic treatment, the inflamed or infected pulp is removed and the inside of the tooth is carefully cleaned and disinfected, then filled and sealed with a rubber-like material called gutta-percha. Afterward, the tooth is restored with a crown or filling for protection and will continue to function like any other tooth.
Endodontic treatment helps you maintain your natural smile, continue eating the foods you love and limits the need for ongoing dental work. With proper care, most teeth that have had root canal treatment can last a lifetime.
For more detailed information on root canal or to organise for a consultation, call us or get in touch online.
Biomimetic Dentistry
What is Biomimetic Dentistry?

Translated literally, biomimetic dentistry means to copy what is life-like. Nature has provided the most successful and ideal properties to our natural teeth. When restoring damaged, broken, and decayed teeth, the goal is to return the tooth to its original strength, function, and esthetics. Biomimetic dentistry accomplishes all of this in a conservative, strong, and attractive approach.
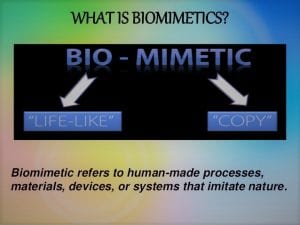
Why is it so important?
Tooth preservation and dental conservation lie at the heart of biomimetic dentistry.
Biomimetic dentistry replicates the strength, function, and aesthetics of natural teeth by replacing only damaged, decayed, and broken tooth structure. The principle employs techniques and materials that provide a perfect balance of nature, art and science.
Teeth move, bend and have physical dynamics of force that must be accounted for while re-making the tooth with nature as our guide. Much of the amputation of tooth structure can be eliminated with modern science. We can say that tooth preservation and dental conservation lie at the heart of biomimetic dentistry.
The economic implications of not needing the advanced, invasive care seen in traditional (amputational) dentistry have profound positive effects on people’s lives. We can now help patients create healthy and happy mouths with simple, and often painless techniques!
Patients are happier and often spend less compared to conventional treatment.
Give us a call to find out more or book a consultation appointment.
Want to stop snoring?
As a condition that affects over 40% of the population, it is no surprise that the majority of us have been impacted by snoring in some way, shape or form. There are both varying degrees and varying types of snoring: it can be ‘simple’, or it can be symptomatic and may require further exploration. Regardless, there are a number of conditions associated, including:
- diminished energy
- lack of concentration
- increased risk of stress
- reduced libido
- high blood pressure
As well as the impact to the snorer, a lack of sleep on the bed partner’s behalf is also dangerous for their health and well-being. Many cases are reported by the bed-partner, with the snorer having very little awareness of their bedtime activities.

Thankfully, there are many interventions that can assist with snoring. Before discussing these, however, it is first important to highlight the cause.
What causes snoring?
Once we are asleep, our muscles relax. This can result in the soft tissues in the throat vibrating, causing the familiar snoring sound.
However, this doesn’t happen to everyone: there are a number of factors that can increase chances of snoring, including: obesity, gender, age, alcohol, and medication. For most sufferers, snoring occurs in isolation (simple snoring). In these cases, it is often the bed-partner that suffers, with the snorer unaware that they are causing such a disturbance. However, it can also take place as part of a more serious condition, obstructive sleep apnoea, which can be potentially life-threatening if not treated correctly.
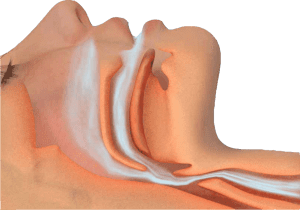
What is obstructive sleep apnoea (OSA)?
OSA is a serious condition where, for short periods of time, the airway becomes blocked during sleep, cutting off oxygen reaching the lungs. There are two types of breathing disruption associated with OSA:
- Apnoea – where the muscles collapse sufficiently enough to cause a total blockage of the airway for 10 seconds or more
- Hypopnoea – partial blockage of the airway that causes an airflow reduction of more than 50% for 10 seconds or more
Both of these problems can occur several times throughout the night and are most commonly recognised by loud snoring, paired with snorts, gasps, or laboured breathing. This leads to disruption for both the bed-partner AND the sufferer, with the snorer often waking feeling tired due to a night with reduced oxygen intake.
There are many associations with obstructive sleep apnoea, and, due to fat distribution, middle-aged males are twice as likely to suffer from OSA in comparison to middle-aged females. The discrepancy does start to level out, however, believed to be due to hormonal changes after menopause.
What are the treatments for snoring?
Though many snorers and tired bed-partners typically look to their doctor for help when it comes to snoring, their dentist arguably has a larger part to play – initially at least.
As snoring is typically caused by the lower jaw dropping back during sleep, the easiest way to stop it is to prevent the jaw from slipping backwards. This can be achieved with a device called a Mandibular Advancement Splint (MAS). Available from trained dentists, there are a number of devices available, one of which is the Sleepwell.

The most clinically proven MAS for the treatment of snoring & mild to moderate sleep apnoea, the Sleepwell is a two-piece device that is fully-adjustable by the wearer, and designed to hold your lower jaw forward. Holistically, however, there may be other behaviours that could assist with the problem, such as:
- Sleeping position – lying on your back inevitably is the worst position for snoring. Trying different positions may have a positive effect.
- Bed-time ‘hygiene’ – avoiding alcohol or caffeine in the evenings can help. Both muscle relaxants, they can increase the chances of snoring.
- Weight-loss – holding excess fat around your neck can play a major role in both snoring and sleep apnoea.
National Stop Snoring Week 23-27 April 2018
Cosmetic Dentistry- What You Should Know

Cosmetic dentistry has become increasingly popular, largely as a result of social trends and increased media coverage. This understandable desire for the alleged ‘perfect smile’ needs to be tempered with an appropriate awareness of the significant risks associated with invasive cosmetic procedures such as veneers and crowns. Patients need to be properly informed that elective removal of healthy enamel and dentine can result in pulpal injury and poorer periodontal health in the longer term, particularly if they are young. The duty of candour means that they ought to be informed that aggressive reduction of sound tooth tissue is not biologically neutral and results in structural weakening of their teeth. Less invasive procedures such as bleaching on its own or for example, combined with direct resin composite bonding, can satisfy many patient’s demands, while still being kinder to teeth and having much better fall-back positions for their future requirements. It is the opinion of the British Endodontic Society, British Society for Restorative Dentistry, Restorative Dentistry UK, Dental Trauma UK, British Society of Prosthodontics and the British Society of Paediatric Dentistry that elective invasive cosmetic dental treatments can result in great benefit to patients, but that some aggressive treatments used to achieve them can produce significant morbidities in teeth which were previously healthy. This is a worrying and growing problem with many ethical, legal and biologic aspects, but many adverse outcomes for patients who request cosmetic dental improvements are preventable by using biologically safer initial approaches to treatment planning and its provision.
Mouth Cancer Awareness Month

Most people have heard of cancer affecting parts of the body such as the lungs or breasts. However, cancer can also occur in the mouth, where the disease can affect the lips, tongue, cheeks and throat.
Anyone can be affected by mouth cancer, whether they have their own teeth or not. Mouth cancers are more common in people over 40, particularly men. However, research has shown that mouth cancer is becoming more common in younger patients and in women. In the last year more than 7,000 have been diagnosed with mouth cancer in the UK – an increase of more than a third compared to a decade ago.
Sadly, more than 1,800 people in the UK lose their life to mouth cancer every year. Many of these deaths could be prevented if the cancer was caught early enough. As it is, people with mouth cancer are more likely to die than those having cervical cancer or melanoma skin cancer.
Find out more at http://www.mouthcancer.org
Teeth whitening
Teeth whitening can be safe when done under the guidance of a dental professional or by following the instructions of over-the-counter products. However, it’s important to be aware of potential side effects, such as tooth sensitivity or gum irritation. Consult your dentist to discuss the best and safest whitening options for your specific needs.
Methods of teeth whitening:
**Professional Whitening:**This is done by a dentist and is the most effective method. It can involve in-office treatments using strong bleaching agents or custom-fitted trays with professional-grade whitening gels.
**Over-the-Counter (OTC) Products:** These include whitening toothpaste, strips, and gels. They are less potent than professional treatments and may take longer to show results.
Benefits of teeth whitening:
Improved Aesthetics: Whitening can remove stains and discoloration, enhancing the appearance of your teeth.
Boosted Confidence: A brighter smile often leads to increased self-confidence.
Non-Invasive: It’s a non-surgical and minimally invasive cosmetic dental procedure.
Risks and considerations:
Tooth Sensitivity: Whitening can cause temporary sensitivity to hot or cold foods and beverages.
Gum Irritation: Overuse or improper application of whitening products can irritate the gums.
Uneven Results: Whitening may not be equally effective on all teeth, leading to uneven results.
Duration of Effect: The duration of whitening effects varies; it may require touch-ups to maintain results.
Pre-existing Dental Issues: Whitening may not be suitable for everyone, especially those with dental restorations (crowns, fillings) as they do not respond to whitening treatments.
It’s crucial to consult with a dentist to discuss your specific needs and any potential risks associated with teeth whitening. They can help you choose the most appropriate and safe method for your situation.
Whitening Toothpastes; Facts and Fallacies
A Guide to Whitening Toothpastes in the UK: Efficacy Backed by Clinical Evidence
Whitening toothpastes are a popular choice for enhancing smiles, but how effective are they? In this blog, we’ll explore different types of whitening toothpastes available in the UK and evaluate their efficacy based on clinical evidence.
Abrasive-Based Whitening Toothpastes
These use mild abrasives like silica to remove surface stains caused by food, drinks, or smoking. While they can visibly improve brightness, clinical studies show they only remove extrinsic stains without altering the tooth’s natural color.
Efficacy: Effective for surface stain removal but not for deeper discoloration.
Enzyme-Based Whitening Toothpastes
Enzyme-based formulations (e.g., containing papain or bromelain) target protein pellicles that cause staining. Evidence suggests they can enhance stain removal without excessive abrasion, making them suitable for sensitive teeth.
Efficacy: Moderate improvement in surface brightness with minimal damage to enamel.
Peroxide-Based Whitening Toothpastes
Some toothpastes contain low levels of hydrogen or carbamide peroxide. Studies indicate they can help lighten intrinsic stains with consistent use over weeks. However, their whitening effect is less significant compared to professional bleaching.
Efficacy: Proven for mild intrinsic whitening, though results are subtle.
Charcoal Whitening Toothpastes
Charcoal-based products are widely marketed for whitening, but clinical evidence shows limited efficacy in removing stains. Excessive use may even harm enamel and gums due to high abrasiveness.
Efficacy: Poor stain removal with potential enamel damage.
Blue Covarine-Infused Toothpastes
These provide an immediate optical effect by depositing a blue pigment on teeth, creating the illusion of whiteness. While the results are temporary, studies support their effectiveness for a quick enhancement.
Efficacy: Temporary improvement in tooth brightness, ideal for short-term use.
Key Takeaways
Best for Surface Stains: Abrasive or enzyme-based toothpastes.
For Intrinsic Whitening: Peroxide-based formulas are most effective but offer mild results.
Quick Fix: Blue covarine toothpastes.
Avoid Overuse: Charcoal toothpastes due to abrasiveness.
For significant whitening or intrinsic stains, professional treatments remain the gold standard. Always consult your dentist to ensure the safest and most effective solution for your smile.
Dental Care and Coronavirus (COVID-19)
It is likely that the coronavirus will have an effect on your dental care.
Routine dental check-ups have been cancelled, and ongoing treatment plans may be disrupted. Where and how you access emergency dental treatment could also change.
This page includes advice on how you can access dental care, treatment and advice during the coronavirus pandemic.
Visiting the dental practice
If you are suffering with your oral health and need support, we are here to help.
To help stop the spread of coronavirus, we are advising against all routine and non-urgent dental treatment.
This includes:
Dental check-ups.
Preventive treatments such as scale and polish and fluoride varnishes.
Examinations and x-rays.
Appointments for braces.
Cosmetic dental treatment of any kind e.g. tooth whitening.
Routine denture treatment.
Treatments on teeth that are not painful e.g. fillings and extractions.
It is likely that your dental practice will contact you to postpone these appointments. If you do not hear from your dental practice, we recommend that you contact them to cancel your appointment and rearrange it for a later date.
In accordance to the instructions received by Public Health England (PHE) and CQC, all dental practices in England have temporarily ceased routine and non-urgent dental treatment. For emergency and urgent dental treatment, the dental surgery will provide remote (telephone or video-link) advice and assessment for further referral to the dedicated NHS Urgent Dental Care Centres (UDC) if necessary.
Whenever possible, stay at home and help stop the spread of coronavirus. This includes people of all ages – even if you do not have any symptoms or other health conditions.
Non-necessary dental treatment is not a reason for you to leave the home.
Urgent Dental Care
The NHS England has set up dedicated Urgent Dental Care Centres (UDC) for emergency and urgent dental conditions. Please note that this is not a walk-in service and requires appropriate referral by your dentist following remote triage.
If you are in pain, bleeding, swelling, or have had an accident and need urgent dental care, please contact your dental practice.
Please do not visit your dental practice without calling them first.
If you are not registered with any dental practice, please call 111 for further advice.
Dental Treatments in hospitals and A&E
To support NHS services and protect vital resources, it is important that you do not visit hospitals or A&E departments with dental problems.
If you need urgent or emergency dental treatment, contact your dental practice and they will be able to triage and direct you.
Dental care for vulnerable people and those with symptoms
If you need urgent dental care and are self-isolating because you have symptoms relating to coronavirus, or are a vulnerable person at higher risk, call NHS 111 or your dental practice.
The dental practice will be able to assess your needs and if necessary refer you to a special team/centre who will be able to treat you.
Buying oral health products
There is no shortage of oral health products like toothbrushes, toothpaste and mouthwash. Because of this, there is no need to stockpile them.
It is important to only buy what you need, when you need it.
Supermarkets remain open for essential food shopping and we advise that you buy any oral health products you need during this time. Please remember however to keep to social distancing rules and maintain two metres away from other shoppers.
When possible, instead of visiting supermarkets, we recommend that you buy oral health products online and have them delivered to your home.
Tips for good oral health
To help prevent dental problems from happening during coronavirus, here are some top tips for good oral health.
- Brush your teeth for two minutes, twice a day with a fluoride toothpaste.
- Do not share your toothbrushes. Keep the toothbrush clean and replace them frequently.
- The best time to brush is first thing in the morning and last thing at night before you go to bed.
- Cut down on how much sugar you have and how often you have it. This is even more important for children at home with increased temptation to snack and consume high sugar diet.
- Keep sugar consumption to mealtimes. This will reduce the time your teeth are under acid -attack.
- Maintain good hydration and avoid smoking and excessive consumption of alcohol.
- Use interdental brushes or floss to clean in between the teeth.
- Use non-alcohol based mouthwash daily to remove bad bacteria and keep fresh breath.
- Sugar-free chewing gum can help produce saliva and neutralise the plaque acids in your mouth.
More information and advice
Children coronavirus fact sheet, click here
For information about the coronavirus (COVID-19), please visit www.nhs.uk/conditions/coronavirus-covid-19/
The desire for the perfect Hollywood smile but at what cost?!

Cosmetic dentistry has become increasingly popular, largely as a result of social trends and increased media coverage. With the reality TV stars setting the trend in an industry now worth £2 billion, this understandable desire for the alleged ‘perfect smile’ needs to be tempered with an appropriate awareness of the significant risks associated with invasive cosmetic procedures such as veneers and crowns.
Patients need to be properly informed that elective removal of healthy enamel and dentine can result in pulpal injury and poorer periodontal health in the longer term, particularly if they are young. The duty of candour means that they ought to be informed that aggressive reduction of sound tooth tissue is not biologically neutral and results in structural weakening of their teeth. Less invasive procedures such as bleaching on its own or for example, combined with direct resin composite bonding, can satisfy many patient’s demands, while still being kinder to teeth and having much better fall-back positions for their future requirements.
It is the opinion of the British Endodontic Society, British Society for Restorative Dentistry, Restorative Dentistry UK, Dental Trauma UK, British Society of Prosthodontics and the British Society of Paediatric Dentistry that elective invasive cosmetic dental treatments can result in great benefit to patients, but that some aggressive treatments used to achieve them can produce significant morbidities in teeth which were previously healthy. This is a worrying and growing problem with many ethical, legal and biologic aspects, but many adverse outcomes for patients who request cosmetic dental improvements are preventable by using biologically safer initial approaches to treatment planning and its provision.
Dedicated personal, specialist care
The Specialist Dental Practice is the leading specialist restorative and implant dental practice in the county and has been setting the standards of specialist dentistry over the last 25 years.
The practice was established in 1973 and is conveniently located in the heart of Weybridge, Surrey. We are UK qualified and registered multi-specialist team offering specialist dental care of the highest quality and precision for the complex reconstruction cases involving dental implant therapy, gum disease treatment, root canal treatment, restoration of mutilated dentition and addressing challenges associated with partial and complete removable dentures.
We are delighted to welcome new referrals to our practice from both patients as well as professional colleagues.
Dental Implants
Essential questions to ask your dentist on dental implants
Taking the decision to have dental implants treatment is something most people will wish to consider quite carefully. Although this treatment can be an excellent long-term solution, it isn’t right for everybody and it is important to have a good understanding of exactly what is required. We have outlined a few essential questions and points you should be aware of before making your final decision.
WHAT ARE YOUR QUALIFICATIONS AND EXPERIENCE IN PLACING DENTAL IMPLANTS?
This is the most important question to ask and should be top of your list. Some clinicians have minimal training in placing dental implants and may only carry out this type of surgery a few times a year.
Our specialist care is based on dental specialties that are officially recognised by the General Dental Council UK. All accredited dental specialists are listed on the General Dental Council website www.gdc-uk.org. The specialist lists exist to:
• ensure high standards of training and assessment qualifying dentists to use a specialist title;
• indicate those dentists who possess recognised specialist knowledge, skills and attitudes;
• protect patients against unwarranted claims to be a specialist;
• facilitate appropriate referrals of patients;
• promote high standards of care by dentists qualified to use a specialist title; and
• encourage postgraduate education.
This list helps patients make an informed decision when they are looking for appropriately trained dentists to manage their dental care.
WHICH IMPLANT SYSTEMS DO YOU USE?
There are a few major dental implant companies that produce high-quality dental implants backed by years of research. These companies are well-known and well respected within the dental industry. There are numerous other companies that produce generic dental implants.
While these may still be of an acceptable quality, they lack the provenance of more widely known dental implant systems. There is another benefit of choosing dental implants made by one of the major companies as these implants are used worldwide. When you need an implant repaired or a component replaced or maintained, it is much easier to find a dentist willing to do this for you, no matter where you are in the world.
DO YOU PROVIDE COMPUTER GUIDED DENTAL IMPLANTS?
Computer guided dental implants surgery involves precisely planning using advanced diagnostics that include a cone beam CT scan and planning software. Once everything is planned, this computerised information is used to create a surgical guide or stent which allows precise placement of each implant.
We prefer to execute guided surgery where possible as it ensures your implant surgery is smoother, quicker and ultimately more comfortable and successful. Not all dentists will use this technique, but it is especially important when placing multiple implants where precision placement is even more vital.
Research shows that appropriately and precisely placed dental implants are less likely to have any problems and complications.
WILL IMPLANT SURGERY HURT?
You should not feel any pain during surgery based on effective local anaesthesia. We know many patients feel anxious at the thought of any oral surgery and if this applies to you then we can discuss additional sedation.
Our dental team is also very experienced at helping nervous patients feel at ease. Most of our patients will report no or very minimal discomfort that is very well managed with simple painkillers following implant surgery.
WILL I NEED A LONG TIME TO RECOVER AFTER IMPLANT SURGERY?
If you need just a single dental implant, you should be back to work the very next day. If you have multiple dental implants you might need a bit longer to recover; your dental implant dentist can give you more advice based on your situation.
Although you may feel some minor discomfort once the anaesthesia wears off, it is not uncommon to feel perfectly fine, especially after single dental implant placements. Again, this is something that can be discussed during your first consultation as it will depend on your treatment.
HOW LONG WILL IT TAKE TO COMPLETE IMPLANT TREATMENT?
Dental implant treatment can take up to several months to complete, as the surgery must be planned and once in place the implants need time to heal. It generally takes about 8-12 weeks for the dental implants to fully heal and to integrate with your jawbone, and the crown or bridge can be placed shortly after. Treatment may take slightly longer if you need bone grafts or tissue regeneration.
WILL I BE LEFT WITHOUT TEETH DURING IMPLANT HEALING?
This is a major concern for many people but there is no need to worry as temporary teeth can be provided while your implants heal. These temporary restorations can be fabricated before your implant surgery and may be placed immediately after surgery is completed.
WILL MY NEW IMPLANT TEETH LOOK NATURAL?
It is essential that your dental implants are placed in precisely the right position for the best functional and aesthetic effects. Here, at The Specialist dental Practice, our team are specialists in restoring and replacing missing teeth with crowns, bridges and dentures to the highest standards ensuring your new teeth are designed to look and feel wonderful. We also offer aftercare and advice on how to keep your implants clean.
HOW CAN I STOP MY DENTAL IMPLANTS FROM FAILING?
While some implants will fail naturally, a large part of implant success comes down to two factors:
• How well the implant is placed and the correct positioning in the jaw
• How well the implant is cared for after placement
Choosing a qualified and skilled implant dentist who is able to plan the correct positioning for your dental implants is key. Whilst you may think a general dentist is slightly cheaper, you may end up paying more in the future with implants that have not been placed correctly with significant potential complications.
The biggest misconception from dental implant patients is that once your dental implants are placed they will be there for life and are indestructible. The fact is, you will need to take care of your dental implants and make sure you regularly attend check-ups and clean your implants properly. Without this, your implants will have a larger chance of failing, both in a biologic and hardware sense.
SHOULD I GO ABROAD TO HAVE DENTAL IMPLANTS?
Dental tourism’ is a concept that has become increasingly popular over the last decade. Patients seek out dental treatment such as dental implants abroad and travel for the sole purpose of receiving cosmetic and restorative dentistry. The main attraction for patients is the cost of treatment in some other countries – it can look like prices are significantly cheaper, depending on the individual treatments. However, as with many things in life, what looks too good to be true often is. There are all kinds of hidden costs with choosing to get dental implants abroad including the prohibitive costs to fix a failing dental implant placed abroad, variation in the standard of care, and lack of long- term aftercare and maintenance plan.
Should you wish to seek more information on dental implant therapy, please contact the practice on 01932857585 or get in touch online info@weybridgedentist.co.uk to arrange for a consultation. In that way, we can assess for your individual needs and provide you with a customised treatment plan .
Specialist treatment for gum disease affecting teeth and dental implants

Understanding the importance of gum health
Gum disease affects many aspects of our life but is often overlooked as it has few symptoms in its early stages – that’s why it is often called ‘the silent disease’.
The vital thing about gum disease is that it is highly preventable and, especially in the early stages, quite easily treatable. Many studies link oral health to a number of significant conditions. There is strong evidence of the links between diabetes and gum disease. For Alzheimer’s and cardio health the role of gum disease is less clear. More than 45% of adults in the UK are affected by gum disease and, even at its most mild level, it can affect your quality of life.
Gum disease can affect dental implants as much as natural teeth. If you have any concerns about your dentition, speak to us and we will be happy to work with your dentist in managing your case.
Saving Your Natural Tooth
Specialist Endodontic Treatment
Nothing looks, feels or functions like your natural teeth, and endodontists are the experts in saving teeth. Keep smiling and eating the foods you love with endodontic treatment that can relieve your pain and save your teeth.
Sometimes your teeth may have infection or disease and will need additional care. When possible, you should always consider treatments to save your teeth. You may think, why not have a tooth pulled, especially if no one can see it, but you will know your tooth is missing and it will negatively impact your quality of life.
Don’t get a tooth pulled because you think its easier or more cost-effective. Missing teeth can cause other teeth to shift, affect your ability to properly chew and ruin your smile. Tooth extraction often is more painful than the infection itself, and replacing an extracted tooth with an artificial one requires additional dental visits that can quickly add up.
Modern endodontics offers advancements in technologies, procedures and materials, giving you many treatment options to save your natural teeth. It’s important to understand your choices and how they’ll impact both your tooth and your future dental health. It’s always best to retain your natural teeth whenever possible and endodontic treatment should be your first choice for the best health and cosmetic results. Endodontists are specialists in saving teeth. They can evaluate your condition and provide the best treatment plan to help you save your teeth for a lifetime.
Here are some tips for saving your teeth:
- When given a choice between tooth extraction and root canal treatment, always opt for a root canal. No denture, bridge or implant will look, feel and function as well as a natural tooth.
- Act immediately when you experience symptoms of swelling or pain. Most endodontists can accommodate emergency cases, even on weekends, ensuring you’ll be seen quickly.
- If your dentist recommends tooth extraction, ask whether the root canal is an option.If you’re told root canal is not an option, ask why and request a referral to an endodontist.
Root canal treatment from an endodontist is virtually painless and often leaves you with less discomfort during recovery than if you have your natural tooth extracted. Thanks to modern techniques and effective anesthesia, patients who experience root canals are six times more likely to describe it as painless than patients who have a tooth extracted! Take the time to learn more about root canal treatment and some of the common misconceptions about it and then take the first step to a pain-free, healthy mouth by visiting an endodontist.
How does endodontic treatment save the tooth?
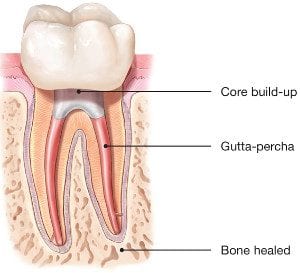
It’s necessary to have endodontic or root canal treatment when the inside of your tooth (the pulp) becomes inflamed or infected as a result of deep decay, repeated dental procedures, faulty crowns or a crack or chip in the tooth. Trauma to your tooth may also cause pulp damage even if the tooth has no visible chips or cracks. If pulp inflammation or infection is left untreated, it can cause pain or lead to an abscess.
When you undergo a root canal or other endodontic treatment, the inflamed or infected pulp is removed and the inside of the tooth is carefully cleaned and disinfected, then filled and sealed with a rubber-like material called gutta-percha. Afterward, the tooth is restored with a crown or filling for protection and will continue to function like any other tooth.
Endodontic treatment helps you maintain your natural smile, continue eating the foods you love and limits the need for ongoing dental work. With proper care, most teeth that have had root canal treatment can last a lifetime.
For more detailed information on root canal or to organise for a consultation, call us or get in touch online.
Biomimetic Dentistry
What is Biomimetic Dentistry?

Translated literally, biomimetic dentistry means to copy what is life-like. Nature has provided the most successful and ideal properties to our natural teeth. When restoring damaged, broken, and decayed teeth, the goal is to return the tooth to its original strength, function, and esthetics. Biomimetic dentistry accomplishes all of this in a conservative, strong, and attractive approach.
Why is it so important?
Tooth preservation and dental conservation lie at the heart of biomimetic dentistry.
Biomimetic dentistry replicates the strength, function, and aesthetics of natural teeth by replacing only damaged, decayed, and broken tooth structure. The principle employs techniques and materials that provide a perfect balance of nature, art and science.
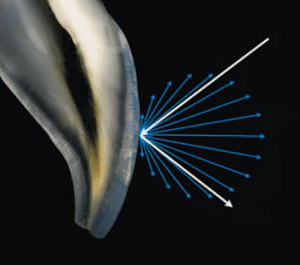
Teeth move, bend and have physical dynamics of force that must be accounted for while re-making the tooth with nature as our guide. Much of the amputation of tooth structure can be eliminated with modern science. We can say that tooth preservation and dental conservation lie at the heart of biomimetic dentistry.
The economic implications of not needing the advanced, invasive care seen in traditional (amputational) dentistry have profound positive effects on people’s lives. We can now help patients create healthy and happy mouths with simple, and often painless techniques!
Patients are happier and often spend less compared to conventional treatment.
Give us a call to find out more or book a consultation appointment.
Want to stop snoring?
As a condition that affects over 40% of the population, it is no surprise that the majority of us have been impacted by snoring in some way, shape or form. There are both varying degrees and varying types of snoring: it can be ‘simple’, or it can be symptomatic and may require further exploration. Regardless, there are a number of conditions associated, including:
- diminished energy
- lack of concentration
- increased risk of stress
- reduced libido
- high blood pressure
As well as the impact to the snorer, a lack of sleep on the bed partner’s behalf is also dangerous for their health and well-being. Many cases are reported by the bed-partner, with the snorer having very little awareness of their bedtime activities.

Thankfully, there are many interventions that can assist with snoring. Before discussing these, however, it is first important to highlight the cause.
What causes snoring?
Once we are asleep, our muscles relax. This can result in the soft tissues in the throat vibrating, causing the familiar snoring sound.
However, this doesn’t happen to everyone: there are a number of factors that can increase chances of snoring, including: obesity, gender, age, alcohol, and medication. For most sufferers, snoring occurs in isolation (simple snoring). In these cases, it is often the bed-partner that suffers, with the snorer unaware that they are causing such a disturbance. However, it can also take place as part of a more serious condition, obstructive sleep apnoea, which can be potentially life-threatening if not treated correctly.
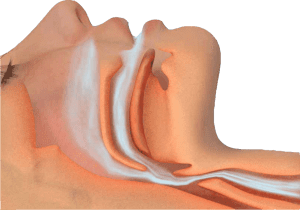
What is obstructive sleep apnoea (OSA)?
OSA is a serious condition where, for short periods of time, the airway becomes blocked during sleep, cutting off oxygen reaching the lungs. There are two types of breathing disruption associated with OSA:
- Apnoea – where the muscles collapse sufficiently enough to cause a total blockage of the airway for 10 seconds or more
- Hypopnoea – partial blockage of the airway that causes an airflow reduction of more than 50% for 10 seconds or more
Both of these problems can occur several times throughout the night and are most commonly recognised by loud snoring, paired with snorts, gasps, or laboured breathing. This leads to disruption for both the bed-partner AND the sufferer, with the snorer often waking feeling tired due to a night with reduced oxygen intake.
There are many associations with obstructive sleep apnoea, and, due to fat distribution, middle-aged males are twice as likely to suffer from OSA in comparison to middle-aged females. The discrepancy does start to level out, however, believed to be due to hormonal changes after menopause.
What are the treatments for snoring?
Though many snorers and tired bed-partners typically look to their doctor for help when it comes to snoring, their dentist arguably has a larger part to play – initially at least.
As snoring is typically caused by the lower jaw dropping back during sleep, the easiest way to stop it is to prevent the jaw from slipping backwards. This can be achieved with a device called a Mandibular Advancement Splint (MAS). Available from trained dentists, there are a number of devices available, one of which is the Sleepwell.

The most clinically proven MAS for the treatment of snoring & mild to moderate sleep apnoea, the Sleepwell is a two-piece device that is fully-adjustable by the wearer, and designed to hold your lower jaw forward. Holistically, however, there may be other behaviours that could assist with the problem, such as:
- Sleeping position – lying on your back inevitably is the worst position for snoring. Trying different positions may have a positive effect.
- Bed-time ‘hygiene’ – avoiding alcohol or caffeine in the evenings can help. Both muscle relaxants, they can increase the chances of snoring.
- Weight-loss – holding excess fat around your neck can play a major role in both snoring and sleep apnoea.
National Stop Snoring Week 23-27 April 2018
Cosmetic Dentistry- What You Should Know

Cosmetic dentistry has become increasingly popular, largely as a result of social trends and increased media coverage. This understandable desire for the alleged ‘perfect smile’ needs to be tempered with an appropriate awareness of the significant risks associated with invasive cosmetic procedures such as veneers and crowns. Patients need to be properly informed that elective removal of healthy enamel and dentine can result in pulpal injury and poorer periodontal health in the longer term, particularly if they are young. The duty of candour means that they ought to be informed that aggressive reduction of sound tooth tissue is not biologically neutral and results in structural weakening of their teeth. Less invasive procedures such as bleaching on its own or for example, combined with direct resin composite bonding, can satisfy many patient’s demands, while still being kinder to teeth and having much better fall-back positions for their future requirements. It is the opinion of the British Endodontic Society, British Society for Restorative Dentistry, Restorative Dentistry UK, Dental Trauma UK, British Society of Prosthodontics and the British Society of Paediatric Dentistry that elective invasive cosmetic dental treatments can result in great benefit to patients, but that some aggressive treatments used to achieve them can produce significant morbidities in teeth which were previously healthy. This is a worrying and growing problem with many ethical, legal and biologic aspects, but many adverse outcomes for patients who request cosmetic dental improvements are preventable by using biologically safer initial approaches to treatment planning and its provision.
Mouth Cancer Awareness Month

Most people have heard of cancer affecting parts of the body such as the lungs or breasts. However, cancer can also occur in the mouth, where the disease can affect the lips, tongue, cheeks and throat.
Anyone can be affected by mouth cancer, whether they have their own teeth or not. Mouth cancers are more common in people over 40, particularly men. However, research has shown that mouth cancer is becoming more common in younger patients and in women. In the last year more than 7,000 have been diagnosed with mouth cancer in the UK – an increase of more than a third compared to a decade ago.
Sadly, more than 1,800 people in the UK lose their life to mouth cancer every year. Many of these deaths could be prevented if the cancer was caught early enough. As it is, people with mouth cancer are more likely to die than those having cervical cancer or melanoma skin cancer.
Find out more at http://www.mouthcancer.org
Teeth whitening
Teeth whitening can be safe when done under the guidance of a dental professional or by following the instructions of over-the-counter products. However, it’s important to be aware of potential side effects, such as tooth sensitivity or gum irritation. Consult your dentist to discuss the best and safest whitening options for your specific needs.
Methods of teeth whitening:
**Professional Whitening:**This is done by a dentist and is the most effective method. It can involve in-office treatments using strong bleaching agents or custom-fitted trays with professional-grade whitening gels.
**Over-the-Counter (OTC) Products:** These include whitening toothpaste, strips, and gels. They are less potent than professional treatments and may take longer to show results.
Benefits of teeth whitening:
Improved Aesthetics: Whitening can remove stains and discoloration, enhancing the appearance of your teeth.
Boosted Confidence: A brighter smile often leads to increased self-confidence.
Non-Invasive: It’s a non-surgical and minimally invasive cosmetic dental procedure.
Risks and considerations:
Tooth Sensitivity: Whitening can cause temporary sensitivity to hot or cold foods and beverages.
Gum Irritation: Overuse or improper application of whitening products can irritate the gums.
Uneven Results: Whitening may not be equally effective on all teeth, leading to uneven results.
Duration of Effect: The duration of whitening effects varies; it may require touch-ups to maintain results.
Pre-existing Dental Issues: Whitening may not be suitable for everyone, especially those with dental restorations (crowns, fillings) as they do not respond to whitening treatments.
It’s crucial to consult with a dentist to discuss your specific needs and any potential risks associated with teeth whitening. They can help you choose the most appropriate and safe method for your situation.
Whitening Toothpastes; Facts and Fallacies
A Guide to Whitening Toothpastes in the UK: Efficacy Backed by Clinical Evidence
Whitening toothpastes are a popular choice for enhancing smiles, but how effective are they? In this blog, we’ll explore different types of whitening toothpastes available in the UK and evaluate their efficacy based on clinical evidence.
Abrasive-Based Whitening Toothpastes
These use mild abrasives like silica to remove surface stains caused by food, drinks, or smoking. While they can visibly improve brightness, clinical studies show they only remove extrinsic stains without altering the tooth’s natural color.
Efficacy: Effective for surface stain removal but not for deeper discoloration.
Enzyme-Based Whitening Toothpastes
Enzyme-based formulations (e.g., containing papain or bromelain) target protein pellicles that cause staining. Evidence suggests they can enhance stain removal without excessive abrasion, making them suitable for sensitive teeth.
Efficacy: Moderate improvement in surface brightness with minimal damage to enamel.
Peroxide-Based Whitening Toothpastes
Some toothpastes contain low levels of hydrogen or carbamide peroxide. Studies indicate they can help lighten intrinsic stains with consistent use over weeks. However, their whitening effect is less significant compared to professional bleaching.
Efficacy: Proven for mild intrinsic whitening, though results are subtle.
Charcoal Whitening Toothpastes
Charcoal-based products are widely marketed for whitening, but clinical evidence shows limited efficacy in removing stains. Excessive use may even harm enamel and gums due to high abrasiveness.
Efficacy: Poor stain removal with potential enamel damage.
Blue Covarine-Infused Toothpastes
These provide an immediate optical effect by depositing a blue pigment on teeth, creating the illusion of whiteness. While the results are temporary, studies support their effectiveness for a quick enhancement.
Efficacy: Temporary improvement in tooth brightness, ideal for short-term use.
Key Takeaways
Best for Surface Stains: Abrasive or enzyme-based toothpastes.
For Intrinsic Whitening: Peroxide-based formulas are most effective but offer mild results.
Quick Fix: Blue covarine toothpastes.
Avoid Overuse: Charcoal toothpastes due to abrasiveness.
For significant whitening or intrinsic stains, professional treatments remain the gold standard. Always consult your dentist to ensure the safest and most effective solution for your smile.
Dental Care and Coronavirus (COVID-19)
It is likely that the coronavirus will have an effect on your dental care.
Routine dental check-ups have been cancelled, and ongoing treatment plans may be disrupted. Where and how you access emergency dental treatment could also change.
This page includes advice on how you can access dental care, treatment and advice during the coronavirus pandemic.
Visiting the dental practice
If you are suffering with your oral health and need support, we are here to help.
To help stop the spread of coronavirus, we are advising against all routine and non-urgent dental treatment.
This includes:
Dental check-ups.
Preventive treatments such as scale and polish and fluoride varnishes.
Examinations and x-rays.
Appointments for braces.
Cosmetic dental treatment of any kind e.g. tooth whitening.
Routine denture treatment.
Treatments on teeth that are not painful e.g. fillings and extractions.
It is likely that your dental practice will contact you to postpone these appointments. If you do not hear from your dental practice, we recommend that you contact them to cancel your appointment and rearrange it for a later date.
In accordance to the instructions received by Public Health England (PHE) and CQC, all dental practices in England have temporarily ceased routine and non-urgent dental treatment. For emergency and urgent dental treatment, the dental surgery will provide remote (telephone or video-link) advice and assessment for further referral to the dedicated NHS Urgent Dental Care Centres (UDC) if necessary.
Whenever possible, stay at home and help stop the spread of coronavirus. This includes people of all ages – even if you do not have any symptoms or other health conditions.
Non-necessary dental treatment is not a reason for you to leave the home.
Urgent Dental Care
The NHS England has set up dedicated Urgent Dental Care Centres (UDC) for emergency and urgent dental conditions. Please note that this is not a walk-in service and requires appropriate referral by your dentist following remote triage.
If you are in pain, bleeding, swelling, or have had an accident and need urgent dental care, please contact your dental practice.
Please do not visit your dental practice without calling them first.
If you are not registered with any dental practice, please call 111 for further advice.
Dental Treatments in hospitals and A&E
To support NHS services and protect vital resources, it is important that you do not visit hospitals or A&E departments with dental problems.
If you need urgent or emergency dental treatment, contact your dental practice and they will be able to triage and direct you.
Dental care for vulnerable people and those with symptoms
If you need urgent dental care and are self-isolating because you have symptoms relating to coronavirus, or are a vulnerable person at higher risk, call NHS 111 or your dental practice.
The dental practice will be able to assess your needs and if necessary refer you to a special team/centre who will be able to treat you.
Buying oral health products
There is no shortage of oral health products like toothbrushes, toothpaste and mouthwash. Because of this, there is no need to stockpile them.
It is important to only buy what you need, when you need it.
Supermarkets remain open for essential food shopping and we advise that you buy any oral health products you need during this time. Please remember however to keep to social distancing rules and maintain two metres away from other shoppers.
When possible, instead of visiting supermarkets, we recommend that you buy oral health products online and have them delivered to your home.
Tips for good oral health
To help prevent dental problems from happening during coronavirus, here are some top tips for good oral health.
- Brush your teeth for two minutes, twice a day with a fluoride toothpaste.
- Do not share your toothbrushes. Keep the toothbrush clean and replace them frequently.
- The best time to brush is first thing in the morning and last thing at night before you go to bed.
- Cut down on how much sugar you have and how often you have it. This is even more important for children at home with increased temptation to snack and consume high sugar diet.
- Keep sugar consumption to mealtimes. This will reduce the time your teeth are under acid -attack.
- Maintain good hydration and avoid smoking and excessive consumption of alcohol.
- Use interdental brushes or floss to clean in between the teeth.
- Use non-alcohol based mouthwash daily to remove bad bacteria and keep fresh breath.
- Sugar-free chewing gum can help produce saliva and neutralise the plaque acids in your mouth.
More information and advice
Children coronavirus fact sheet, click here
For information about the coronavirus (COVID-19), please visit www.nhs.uk/conditions/coronavirus-covid-19/
The desire for the perfect Hollywood smile but at what cost?!

Cosmetic dentistry has become increasingly popular, largely as a result of social trends and increased media coverage. With the reality TV stars setting the trend in an industry now worth £2 billion, this understandable desire for the alleged ‘perfect smile’ needs to be tempered with an appropriate awareness of the significant risks associated with invasive cosmetic procedures such as veneers and crowns.
Patients need to be properly informed that elective removal of healthy enamel and dentine can result in pulpal injury and poorer periodontal health in the longer term, particularly if they are young. The duty of candour means that they ought to be informed that aggressive reduction of sound tooth tissue is not biologically neutral and results in structural weakening of their teeth. Less invasive procedures such as bleaching on its own or for example, combined with direct resin composite bonding, can satisfy many patient’s demands, while still being kinder to teeth and having much better fall-back positions for their future requirements.
It is the opinion of the British Endodontic Society, British Society for Restorative Dentistry, Restorative Dentistry UK, Dental Trauma UK, British Society of Prosthodontics and the British Society of Paediatric Dentistry that elective invasive cosmetic dental treatments can result in great benefit to patients, but that some aggressive treatments used to achieve them can produce significant morbidities in teeth which were previously healthy. This is a worrying and growing problem with many ethical, legal and biologic aspects, but many adverse outcomes for patients who request cosmetic dental improvements are preventable by using biologically safer initial approaches to treatment planning and its provision.
Dedicated personal, specialist care
The Specialist Dental Practice is the leading specialist restorative and implant dental practice in the county and has been setting the standards of specialist dentistry over the last 25 years.
The practice was established in 1973 and is conveniently located in the heart of Weybridge, Surrey. We are UK qualified and registered multi-specialist team offering specialist dental care of the highest quality and precision for the complex reconstruction cases involving dental implant therapy, gum disease treatment, root canal treatment, restoration of mutilated dentition and addressing challenges associated with partial and complete removable dentures.
We are delighted to welcome new referrals to our practice from both patients as well as professional colleagues.
Dental Implants
Essential questions to ask your dentist on dental implants
Taking the decision to have dental implants treatment is something most people will wish to consider quite carefully. Although this treatment can be an excellent long-term solution, it isn’t right for everybody and it is important to have a good understanding of exactly what is required. We have outlined a few essential questions and points you should be aware of before making your final decision.
WHAT ARE YOUR QUALIFICATIONS AND EXPERIENCE IN PLACING DENTAL IMPLANTS?
This is the most important question to ask and should be top of your list. Some clinicians have minimal training in placing dental implants and may only carry out this type of surgery a few times a year.
Our specialist care is based on dental specialties that are officially recognised by the General Dental Council UK. All accredited dental specialists are listed on the General Dental Council website www.gdc-uk.org. The specialist lists exist to:
• ensure high standards of training and assessment qualifying dentists to use a specialist title;
• indicate those dentists who possess recognised specialist knowledge, skills and attitudes;
• protect patients against unwarranted claims to be a specialist;
• facilitate appropriate referrals of patients;
• promote high standards of care by dentists qualified to use a specialist title; and
• encourage postgraduate education.
This list helps patients make an informed decision when they are looking for appropriately trained dentists to manage their dental care.
WHICH IMPLANT SYSTEMS DO YOU USE?
There are a few major dental implant companies that produce high-quality dental implants backed by years of research. These companies are well-known and well respected within the dental industry. There are numerous other companies that produce generic dental implants.
While these may still be of an acceptable quality, they lack the provenance of more widely known dental implant systems. There is another benefit of choosing dental implants made by one of the major companies as these implants are used worldwide. When you need an implant repaired or a component replaced or maintained, it is much easier to find a dentist willing to do this for you, no matter where you are in the world.
DO YOU PROVIDE COMPUTER GUIDED DENTAL IMPLANTS?
Computer guided dental implants surgery involves precisely planning using advanced diagnostics that include a cone beam CT scan and planning software. Once everything is planned, this computerised information is used to create a surgical guide or stent which allows precise placement of each implant.
We prefer to execute guided surgery where possible as it ensures your implant surgery is smoother, quicker and ultimately more comfortable and successful. Not all dentists will use this technique, but it is especially important when placing multiple implants where precision placement is even more vital.
Research shows that appropriately and precisely placed dental implants are less likely to have any problems and complications.
WILL IMPLANT SURGERY HURT?
You should not feel any pain during surgery based on effective local anaesthesia. We know many patients feel anxious at the thought of any oral surgery and if this applies to you then we can discuss additional sedation.
Our dental team is also very experienced at helping nervous patients feel at ease. Most of our patients will report no or very minimal discomfort that is very well managed with simple painkillers following implant surgery.
WILL I NEED A LONG TIME TO RECOVER AFTER IMPLANT SURGERY?
If you need just a single dental implant, you should be back to work the very next day. If you have multiple dental implants you might need a bit longer to recover; your dental implant dentist can give you more advice based on your situation.
Although you may feel some minor discomfort once the anaesthesia wears off, it is not uncommon to feel perfectly fine, especially after single dental implant placements. Again, this is something that can be discussed during your first consultation as it will depend on your treatment.
HOW LONG WILL IT TAKE TO COMPLETE IMPLANT TREATMENT?
Dental implant treatment can take up to several months to complete, as the surgery must be planned and once in place the implants need time to heal. It generally takes about 8-12 weeks for the dental implants to fully heal and to integrate with your jawbone, and the crown or bridge can be placed shortly after. Treatment may take slightly longer if you need bone grafts or tissue regeneration.
WILL I BE LEFT WITHOUT TEETH DURING IMPLANT HEALING?
This is a major concern for many people but there is no need to worry as temporary teeth can be provided while your implants heal. These temporary restorations can be fabricated before your implant surgery and may be placed immediately after surgery is completed.
WILL MY NEW IMPLANT TEETH LOOK NATURAL?
It is essential that your dental implants are placed in precisely the right position for the best functional and aesthetic effects. Here, at The Specialist dental Practice, our team are specialists in restoring and replacing missing teeth with crowns, bridges and dentures to the highest standards ensuring your new teeth are designed to look and feel wonderful. We also offer aftercare and advice on how to keep your implants clean.
HOW CAN I STOP MY DENTAL IMPLANTS FROM FAILING?
While some implants will fail naturally, a large part of implant success comes down to two factors:
• How well the implant is placed and the correct positioning in the jaw
• How well the implant is cared for after placement
Choosing a qualified and skilled implant dentist who is able to plan the correct positioning for your dental implants is key. Whilst you may think a general dentist is slightly cheaper, you may end up paying more in the future with implants that have not been placed correctly with significant potential complications.
The biggest misconception from dental implant patients is that once your dental implants are placed they will be there for life and are indestructible. The fact is, you will need to take care of your dental implants and make sure you regularly attend check-ups and clean your implants properly. Without this, your implants will have a larger chance of failing, both in a biologic and hardware sense.
SHOULD I GO ABROAD TO HAVE DENTAL IMPLANTS?
Dental tourism’ is a concept that has become increasingly popular over the last decade. Patients seek out dental treatment such as dental implants abroad and travel for the sole purpose of receiving cosmetic and restorative dentistry. The main attraction for patients is the cost of treatment in some other countries – it can look like prices are significantly cheaper, depending on the individual treatments. However, as with many things in life, what looks too good to be true often is. There are all kinds of hidden costs with choosing to get dental implants abroad including the prohibitive costs to fix a failing dental implant placed abroad, variation in the standard of care, and lack of long- term aftercare and maintenance plan.
Should you wish to seek more information on dental implant therapy, please contact the practice on 01932857585 or get in touch online info@weybridgedentist.co.uk to arrange for a consultation. In that way, we can assess for your individual needs and provide you with a customised treatment plan .
Specialist treatment for gum disease affecting teeth and dental implants

Understanding the importance of gum health
Gum disease affects many aspects of our life but is often overlooked as it has few symptoms in its early stages – that’s why it is often called ‘the silent disease’.
The vital thing about gum disease is that it is highly preventable and, especially in the early stages, quite easily treatable. Many studies link oral health to a number of significant conditions. There is strong evidence of the links between diabetes and gum disease. For Alzheimer’s and cardio health the role of gum disease is less clear. More than 45% of adults in the UK are affected by gum disease and, even at its most mild level, it can affect your quality of life.
Gum disease can affect dental implants as much as natural teeth. If you have any concerns about your dentition, speak to us and we will be happy to work with your dentist in managing your case.
Saving Your Natural Tooth
Specialist Endodontic Treatment
Nothing looks, feels or functions like your natural teeth, and endodontists are the experts in saving teeth. Keep smiling and eating the foods you love with endodontic treatment that can relieve your pain and save your teeth.
Sometimes your teeth may have infection or disease and will need additional care. When possible, you should always consider treatments to save your teeth. You may think, why not have a tooth pulled, especially if no one can see it, but you will know your tooth is missing and it will negatively impact your quality of life.
Don’t get a tooth pulled because you think its easier or more cost-effective. Missing teeth can cause other teeth to shift, affect your ability to properly chew and ruin your smile. Tooth extraction often is more painful than the infection itself, and replacing an extracted tooth with an artificial one requires additional dental visits that can quickly add up.
Modern endodontics offers advancements in technologies, procedures and materials, giving you many treatment options to save your natural teeth. It’s important to understand your choices and how they’ll impact both your tooth and your future dental health. It’s always best to retain your natural teeth whenever possible and endodontic treatment should be your first choice for the best health and cosmetic results. Endodontists are specialists in saving teeth. They can evaluate your condition and provide the best treatment plan to help you save your teeth for a lifetime.
Here are some tips for saving your teeth:
- When given a choice between tooth extraction and root canal treatment, always opt for a root canal. No denture, bridge or implant will look, feel and function as well as a natural tooth.
- Act immediately when you experience symptoms of swelling or pain. Most endodontists can accommodate emergency cases, even on weekends, ensuring you’ll be seen quickly.
- If your dentist recommends tooth extraction, ask whether the root canal is an option.If you’re told root canal is not an option, ask why and request a referral to an endodontist.
Root canal treatment from an endodontist is virtually painless and often leaves you with less discomfort during recovery than if you have your natural tooth extracted. Thanks to modern techniques and effective anesthesia, patients who experience root canals are six times more likely to describe it as painless than patients who have a tooth extracted! Take the time to learn more about root canal treatment and some of the common misconceptions about it and then take the first step to a pain-free, healthy mouth by visiting an endodontist.
How does endodontic treatment save the tooth?
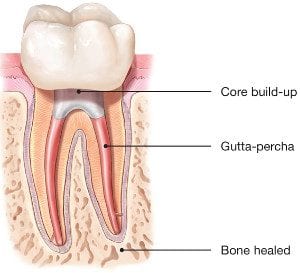
It’s necessary to have endodontic or root canal treatment when the inside of your tooth (the pulp) becomes inflamed or infected as a result of deep decay, repeated dental procedures, faulty crowns or a crack or chip in the tooth. Trauma to your tooth may also cause pulp damage even if the tooth has no visible chips or cracks. If pulp inflammation or infection is left untreated, it can cause pain or lead to an abscess.
When you undergo a root canal or other endodontic treatment, the inflamed or infected pulp is removed and the inside of the tooth is carefully cleaned and disinfected, then filled and sealed with a rubber-like material called gutta-percha. Afterward, the tooth is restored with a crown or filling for protection and will continue to function like any other tooth.
Endodontic treatment helps you maintain your natural smile, continue eating the foods you love and limits the need for ongoing dental work. With proper care, most teeth that have had root canal treatment can last a lifetime.
For more detailed information on root canal or to organise for a consultation, call us or get in touch online.
Biomimetic Dentistry
What is Biomimetic Dentistry?

Translated literally, biomimetic dentistry means to copy what is life-like. Nature has provided the most successful and ideal properties to our natural teeth. When restoring damaged, broken, and decayed teeth, the goal is to return the tooth to its original strength, function, and esthetics. Biomimetic dentistry accomplishes all of this in a conservative, strong, and attractive approach.
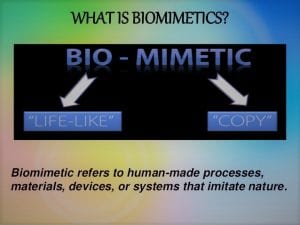
Why is it so important?
Tooth preservation and dental conservation lie at the heart of biomimetic dentistry.
Biomimetic dentistry replicates the strength, function, and aesthetics of natural teeth by replacing only damaged, decayed, and broken tooth structure. The principle employs techniques and materials that provide a perfect balance of nature, art and science.
Teeth move, bend and have physical dynamics of force that must be accounted for while re-making the tooth with nature as our guide. Much of the amputation of tooth structure can be eliminated with modern science. We can say that tooth preservation and dental conservation lie at the heart of biomimetic dentistry.
The economic implications of not needing the advanced, invasive care seen in traditional (amputational) dentistry have profound positive effects on people’s lives. We can now help patients create healthy and happy mouths with simple, and often painless techniques!
Patients are happier and often spend less compared to conventional treatment.
Give us a call to find out more or book a consultation appointment.
Want to stop snoring?
As a condition that affects over 40% of the population, it is no surprise that the majority of us have been impacted by snoring in some way, shape or form. There are both varying degrees and varying types of snoring: it can be ‘simple’, or it can be symptomatic and may require further exploration. Regardless, there are a number of conditions associated, including:
- diminished energy
- lack of concentration
- increased risk of stress
- reduced libido
- high blood pressure
As well as the impact to the snorer, a lack of sleep on the bed partner’s behalf is also dangerous for their health and well-being. Many cases are reported by the bed-partner, with the snorer having very little awareness of their bedtime activities.

Thankfully, there are many interventions that can assist with snoring. Before discussing these, however, it is first important to highlight the cause.
What causes snoring?
Once we are asleep, our muscles relax. This can result in the soft tissues in the throat vibrating, causing the familiar snoring sound.
However, this doesn’t happen to everyone: there are a number of factors that can increase chances of snoring, including: obesity, gender, age, alcohol, and medication. For most sufferers, snoring occurs in isolation (simple snoring). In these cases, it is often the bed-partner that suffers, with the snorer unaware that they are causing such a disturbance. However, it can also take place as part of a more serious condition, obstructive sleep apnoea, which can be potentially life-threatening if not treated correctly.
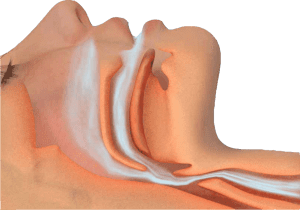
What is obstructive sleep apnoea (OSA)?
OSA is a serious condition where, for short periods of time, the airway becomes blocked during sleep, cutting off oxygen reaching the lungs. There are two types of breathing disruption associated with OSA:
- Apnoea – where the muscles collapse sufficiently enough to cause a total blockage of the airway for 10 seconds or more
- Hypopnoea – partial blockage of the airway that causes an airflow reduction of more than 50% for 10 seconds or more
Both of these problems can occur several times throughout the night and are most commonly recognised by loud snoring, paired with snorts, gasps, or laboured breathing. This leads to disruption for both the bed-partner AND the sufferer, with the snorer often waking feeling tired due to a night with reduced oxygen intake.
There are many associations with obstructive sleep apnoea, and, due to fat distribution, middle-aged males are twice as likely to suffer from OSA in comparison to middle-aged females. The discrepancy does start to level out, however, believed to be due to hormonal changes after menopause.
What are the treatments for snoring?
Though many snorers and tired bed-partners typically look to their doctor for help when it comes to snoring, their dentist arguably has a larger part to play – initially at least.
As snoring is typically caused by the lower jaw dropping back during sleep, the easiest way to stop it is to prevent the jaw from slipping backwards. This can be achieved with a device called a Mandibular Advancement Splint (MAS). Available from trained dentists, there are a number of devices available, one of which is the Sleepwell.

The most clinically proven MAS for the treatment of snoring & mild to moderate sleep apnoea, the Sleepwell is a two-piece device that is fully-adjustable by the wearer, and designed to hold your lower jaw forward. Holistically, however, there may be other behaviours that could assist with the problem, such as:
- Sleeping position – lying on your back inevitably is the worst position for snoring. Trying different positions may have a positive effect.
- Bed-time ‘hygiene’ – avoiding alcohol or caffeine in the evenings can help. Both muscle relaxants, they can increase the chances of snoring.
- Weight-loss – holding excess fat around your neck can play a major role in both snoring and sleep apnoea.
National Stop Snoring Week 23-27 April 2018
Cosmetic Dentistry- What You Should Know

Cosmetic dentistry has become increasingly popular, largely as a result of social trends and increased media coverage. This understandable desire for the alleged ‘perfect smile’ needs to be tempered with an appropriate awareness of the significant risks associated with invasive cosmetic procedures such as veneers and crowns. Patients need to be properly informed that elective removal of healthy enamel and dentine can result in pulpal injury and poorer periodontal health in the longer term, particularly if they are young. The duty of candour means that they ought to be informed that aggressive reduction of sound tooth tissue is not biologically neutral and results in structural weakening of their teeth. Less invasive procedures such as bleaching on its own or for example, combined with direct resin composite bonding, can satisfy many patient’s demands, while still being kinder to teeth and having much better fall-back positions for their future requirements. It is the opinion of the British Endodontic Society, British Society for Restorative Dentistry, Restorative Dentistry UK, Dental Trauma UK, British Society of Prosthodontics and the British Society of Paediatric Dentistry that elective invasive cosmetic dental treatments can result in great benefit to patients, but that some aggressive treatments used to achieve them can produce significant morbidities in teeth which were previously healthy. This is a worrying and growing problem with many ethical, legal and biologic aspects, but many adverse outcomes for patients who request cosmetic dental improvements are preventable by using biologically safer initial approaches to treatment planning and its provision.
Mouth Cancer Awareness Month

Most people have heard of cancer affecting parts of the body such as the lungs or breasts. However, cancer can also occur in the mouth, where the disease can affect the lips, tongue, cheeks and throat.
Anyone can be affected by mouth cancer, whether they have their own teeth or not. Mouth cancers are more common in people over 40, particularly men. However, research has shown that mouth cancer is becoming more common in younger patients and in women. In the last year more than 7,000 have been diagnosed with mouth cancer in the UK – an increase of more than a third compared to a decade ago.
Sadly, more than 1,800 people in the UK lose their life to mouth cancer every year. Many of these deaths could be prevented if the cancer was caught early enough. As it is, people with mouth cancer are more likely to die than those having cervical cancer or melanoma skin cancer.
Find out more at http://www.mouthcancer.org
Teeth whitening
Teeth whitening can be safe when done under the guidance of a dental professional or by following the instructions of over-the-counter products. However, it’s important to be aware of potential side effects, such as tooth sensitivity or gum irritation. Consult your dentist to discuss the best and safest whitening options for your specific needs.
Methods of teeth whitening:
**Professional Whitening:**This is done by a dentist and is the most effective method. It can involve in-office treatments using strong bleaching agents or custom-fitted trays with professional-grade whitening gels.
**Over-the-Counter (OTC) Products:** These include whitening toothpaste, strips, and gels. They are less potent than professional treatments and may take longer to show results.
Benefits of teeth whitening:
Improved Aesthetics: Whitening can remove stains and discoloration, enhancing the appearance of your teeth.
Boosted Confidence: A brighter smile often leads to increased self-confidence.
Non-Invasive: It’s a non-surgical and minimally invasive cosmetic dental procedure.
Risks and considerations:
Tooth Sensitivity: Whitening can cause temporary sensitivity to hot or cold foods and beverages.
Gum Irritation: Overuse or improper application of whitening products can irritate the gums.
Uneven Results: Whitening may not be equally effective on all teeth, leading to uneven results.
Duration of Effect: The duration of whitening effects varies; it may require touch-ups to maintain results.
Pre-existing Dental Issues: Whitening may not be suitable for everyone, especially those with dental restorations (crowns, fillings) as they do not respond to whitening treatments.
It’s crucial to consult with a dentist to discuss your specific needs and any potential risks associated with teeth whitening. They can help you choose the most appropriate and safe method for your situation.
Whitening Toothpastes; Facts and Fallacies
A Guide to Whitening Toothpastes in the UK: Efficacy Backed by Clinical Evidence
Whitening toothpastes are a popular choice for enhancing smiles, but how effective are they? In this blog, we’ll explore different types of whitening toothpastes available in the UK and evaluate their efficacy based on clinical evidence.
Abrasive-Based Whitening Toothpastes
These use mild abrasives like silica to remove surface stains caused by food, drinks, or smoking. While they can visibly improve brightness, clinical studies show they only remove extrinsic stains without altering the tooth’s natural color.
Efficacy: Effective for surface stain removal but not for deeper discoloration.
Enzyme-Based Whitening Toothpastes
Enzyme-based formulations (e.g., containing papain or bromelain) target protein pellicles that cause staining. Evidence suggests they can enhance stain removal without excessive abrasion, making them suitable for sensitive teeth.
Efficacy: Moderate improvement in surface brightness with minimal damage to enamel.
Peroxide-Based Whitening Toothpastes
Some toothpastes contain low levels of hydrogen or carbamide peroxide. Studies indicate they can help lighten intrinsic stains with consistent use over weeks. However, their whitening effect is less significant compared to professional bleaching.
Efficacy: Proven for mild intrinsic whitening, though results are subtle.
Charcoal Whitening Toothpastes
Charcoal-based products are widely marketed for whitening, but clinical evidence shows limited efficacy in removing stains. Excessive use may even harm enamel and gums due to high abrasiveness.
Efficacy: Poor stain removal with potential enamel damage.
Blue Covarine-Infused Toothpastes
These provide an immediate optical effect by depositing a blue pigment on teeth, creating the illusion of whiteness. While the results are temporary, studies support their effectiveness for a quick enhancement.
Efficacy: Temporary improvement in tooth brightness, ideal for short-term use.
Key Takeaways
Best for Surface Stains: Abrasive or enzyme-based toothpastes.
For Intrinsic Whitening: Peroxide-based formulas are most effective but offer mild results.
Quick Fix: Blue covarine toothpastes.
Avoid Overuse: Charcoal toothpastes due to abrasiveness.
For significant whitening or intrinsic stains, professional treatments remain the gold standard. Always consult your dentist to ensure the safest and most effective solution for your smile.
Dental Care and Coronavirus (COVID-19)
It is likely that the coronavirus will have an effect on your dental care.
Routine dental check-ups have been cancelled, and ongoing treatment plans may be disrupted. Where and how you access emergency dental treatment could also change.
This page includes advice on how you can access dental care, treatment and advice during the coronavirus pandemic.
Visiting the dental practice
If you are suffering with your oral health and need support, we are here to help.
To help stop the spread of coronavirus, we are advising against all routine and non-urgent dental treatment.
This includes:
Dental check-ups.
Preventive treatments such as scale and polish and fluoride varnishes.
Examinations and x-rays.
Appointments for braces.
Cosmetic dental treatment of any kind e.g. tooth whitening.
Routine denture treatment.
Treatments on teeth that are not painful e.g. fillings and extractions.
It is likely that your dental practice will contact you to postpone these appointments. If you do not hear from your dental practice, we recommend that you contact them to cancel your appointment and rearrange it for a later date.
In accordance to the instructions received by Public Health England (PHE) and CQC, all dental practices in England have temporarily ceased routine and non-urgent dental treatment. For emergency and urgent dental treatment, the dental surgery will provide remote (telephone or video-link) advice and assessment for further referral to the dedicated NHS Urgent Dental Care Centres (UDC) if necessary.
Whenever possible, stay at home and help stop the spread of coronavirus. This includes people of all ages – even if you do not have any symptoms or other health conditions.
Non-necessary dental treatment is not a reason for you to leave the home.
Urgent Dental Care
The NHS England has set up dedicated Urgent Dental Care Centres (UDC) for emergency and urgent dental conditions. Please note that this is not a walk-in service and requires appropriate referral by your dentist following remote triage.
If you are in pain, bleeding, swelling, or have had an accident and need urgent dental care, please contact your dental practice.
Please do not visit your dental practice without calling them first.
If you are not registered with any dental practice, please call 111 for further advice.
Dental Treatments in hospitals and A&E
To support NHS services and protect vital resources, it is important that you do not visit hospitals or A&E departments with dental problems.
If you need urgent or emergency dental treatment, contact your dental practice and they will be able to triage and direct you.
Dental care for vulnerable people and those with symptoms
If you need urgent dental care and are self-isolating because you have symptoms relating to coronavirus, or are a vulnerable person at higher risk, call NHS 111 or your dental practice.
The dental practice will be able to assess your needs and if necessary refer you to a special team/centre who will be able to treat you.
Buying oral health products
There is no shortage of oral health products like toothbrushes, toothpaste and mouthwash. Because of this, there is no need to stockpile them.
It is important to only buy what you need, when you need it.
Supermarkets remain open for essential food shopping and we advise that you buy any oral health products you need during this time. Please remember however to keep to social distancing rules and maintain two metres away from other shoppers.
When possible, instead of visiting supermarkets, we recommend that you buy oral health products online and have them delivered to your home.
Tips for good oral health
To help prevent dental problems from happening during coronavirus, here are some top tips for good oral health.
- Brush your teeth for two minutes, twice a day with a fluoride toothpaste.
- Do not share your toothbrushes. Keep the toothbrush clean and replace them frequently.
- The best time to brush is first thing in the morning and last thing at night before you go to bed.
- Cut down on how much sugar you have and how often you have it. This is even more important for children at home with increased temptation to snack and consume high sugar diet.
- Keep sugar consumption to mealtimes. This will reduce the time your teeth are under acid -attack.
- Maintain good hydration and avoid smoking and excessive consumption of alcohol.
- Use interdental brushes or floss to clean in between the teeth.
- Use non-alcohol based mouthwash daily to remove bad bacteria and keep fresh breath.
- Sugar-free chewing gum can help produce saliva and neutralise the plaque acids in your mouth.
More information and advice
Children coronavirus fact sheet, click here
For information about the coronavirus (COVID-19), please visit www.nhs.uk/conditions/coronavirus-covid-19/
The desire for the perfect Hollywood smile but at what cost?!

Cosmetic dentistry has become increasingly popular, largely as a result of social trends and increased media coverage. With the reality TV stars setting the trend in an industry now worth £2 billion, this understandable desire for the alleged ‘perfect smile’ needs to be tempered with an appropriate awareness of the significant risks associated with invasive cosmetic procedures such as veneers and crowns.
Patients need to be properly informed that elective removal of healthy enamel and dentine can result in pulpal injury and poorer periodontal health in the longer term, particularly if they are young. The duty of candour means that they ought to be informed that aggressive reduction of sound tooth tissue is not biologically neutral and results in structural weakening of their teeth. Less invasive procedures such as bleaching on its own or for example, combined with direct resin composite bonding, can satisfy many patient’s demands, while still being kinder to teeth and having much better fall-back positions for their future requirements.
It is the opinion of the British Endodontic Society, British Society for Restorative Dentistry, Restorative Dentistry UK, Dental Trauma UK, British Society of Prosthodontics and the British Society of Paediatric Dentistry that elective invasive cosmetic dental treatments can result in great benefit to patients, but that some aggressive treatments used to achieve them can produce significant morbidities in teeth which were previously healthy. This is a worrying and growing problem with many ethical, legal and biologic aspects, but many adverse outcomes for patients who request cosmetic dental improvements are preventable by using biologically safer initial approaches to treatment planning and its provision.
Dedicated personal, specialist care
The Specialist Dental Practice is the leading specialist restorative and implant dental practice in the county and has been setting the standards of specialist dentistry over the last 25 years.
The practice was established in 1973 and is conveniently located in the heart of Weybridge, Surrey. We are UK qualified and registered multi-specialist team offering specialist dental care of the highest quality and precision for the complex reconstruction cases involving dental implant therapy, gum disease treatment, root canal treatment, restoration of mutilated dentition and addressing challenges associated with partial and complete removable dentures.
We are delighted to welcome new referrals to our practice from both patients as well as professional colleagues.
Dental Implants
Essential questions to ask your dentist on dental implants
Taking the decision to have dental implants treatment is something most people will wish to consider quite carefully. Although this treatment can be an excellent long-term solution, it isn’t right for everybody and it is important to have a good understanding of exactly what is required. We have outlined a few essential questions and points you should be aware of before making your final decision.
WHAT ARE YOUR QUALIFICATIONS AND EXPERIENCE IN PLACING DENTAL IMPLANTS?
This is the most important question to ask and should be top of your list. Some clinicians have minimal training in placing dental implants and may only carry out this type of surgery a few times a year.
Our specialist care is based on dental specialties that are officially recognised by the General Dental Council UK. All accredited dental specialists are listed on the General Dental Council website www.gdc-uk.org. The specialist lists exist to:
• ensure high standards of training and assessment qualifying dentists to use a specialist title;
• indicate those dentists who possess recognised specialist knowledge, skills and attitudes;
• protect patients against unwarranted claims to be a specialist;
• facilitate appropriate referrals of patients;
• promote high standards of care by dentists qualified to use a specialist title; and
• encourage postgraduate education.
This list helps patients make an informed decision when they are looking for appropriately trained dentists to manage their dental care.
WHICH IMPLANT SYSTEMS DO YOU USE?
There are a few major dental implant companies that produce high-quality dental implants backed by years of research. These companies are well-known and well respected within the dental industry. There are numerous other companies that produce generic dental implants.
While these may still be of an acceptable quality, they lack the provenance of more widely known dental implant systems. There is another benefit of choosing dental implants made by one of the major companies as these implants are used worldwide. When you need an implant repaired or a component replaced or maintained, it is much easier to find a dentist willing to do this for you, no matter where you are in the world.
DO YOU PROVIDE COMPUTER GUIDED DENTAL IMPLANTS?
Computer guided dental implants surgery involves precisely planning using advanced diagnostics that include a cone beam CT scan and planning software. Once everything is planned, this computerised information is used to create a surgical guide or stent which allows precise placement of each implant.
We prefer to execute guided surgery where possible as it ensures your implant surgery is smoother, quicker and ultimately more comfortable and successful. Not all dentists will use this technique, but it is especially important when placing multiple implants where precision placement is even more vital.
Research shows that appropriately and precisely placed dental implants are less likely to have any problems and complications.
WILL IMPLANT SURGERY HURT?
You should not feel any pain during surgery based on effective local anaesthesia. We know many patients feel anxious at the thought of any oral surgery and if this applies to you then we can discuss additional sedation.
Our dental team is also very experienced at helping nervous patients feel at ease. Most of our patients will report no or very minimal discomfort that is very well managed with simple painkillers following implant surgery.
WILL I NEED A LONG TIME TO RECOVER AFTER IMPLANT SURGERY?
If you need just a single dental implant, you should be back to work the very next day. If you have multiple dental implants you might need a bit longer to recover; your dental implant dentist can give you more advice based on your situation.
Although you may feel some minor discomfort once the anaesthesia wears off, it is not uncommon to feel perfectly fine, especially after single dental implant placements. Again, this is something that can be discussed during your first consultation as it will depend on your treatment.
HOW LONG WILL IT TAKE TO COMPLETE IMPLANT TREATMENT?
Dental implant treatment can take up to several months to complete, as the surgery must be planned and once in place the implants need time to heal. It generally takes about 8-12 weeks for the dental implants to fully heal and to integrate with your jawbone, and the crown or bridge can be placed shortly after. Treatment may take slightly longer if you need bone grafts or tissue regeneration.
WILL I BE LEFT WITHOUT TEETH DURING IMPLANT HEALING?
This is a major concern for many people but there is no need to worry as temporary teeth can be provided while your implants heal. These temporary restorations can be fabricated before your implant surgery and may be placed immediately after surgery is completed.
WILL MY NEW IMPLANT TEETH LOOK NATURAL?
It is essential that your dental implants are placed in precisely the right position for the best functional and aesthetic effects. Here, at The Specialist dental Practice, our team are specialists in restoring and replacing missing teeth with crowns, bridges and dentures to the highest standards ensuring your new teeth are designed to look and feel wonderful. We also offer aftercare and advice on how to keep your implants clean.
HOW CAN I STOP MY DENTAL IMPLANTS FROM FAILING?
While some implants will fail naturally, a large part of implant success comes down to two factors:
• How well the implant is placed and the correct positioning in the jaw
• How well the implant is cared for after placement
Choosing a qualified and skilled implant dentist who is able to plan the correct positioning for your dental implants is key. Whilst you may think a general dentist is slightly cheaper, you may end up paying more in the future with implants that have not been placed correctly with significant potential complications.
The biggest misconception from dental implant patients is that once your dental implants are placed they will be there for life and are indestructible. The fact is, you will need to take care of your dental implants and make sure you regularly attend check-ups and clean your implants properly. Without this, your implants will have a larger chance of failing, both in a biologic and hardware sense.
SHOULD I GO ABROAD TO HAVE DENTAL IMPLANTS?
Dental tourism’ is a concept that has become increasingly popular over the last decade. Patients seek out dental treatment such as dental implants abroad and travel for the sole purpose of receiving cosmetic and restorative dentistry. The main attraction for patients is the cost of treatment in some other countries – it can look like prices are significantly cheaper, depending on the individual treatments. However, as with many things in life, what looks too good to be true often is. There are all kinds of hidden costs with choosing to get dental implants abroad including the prohibitive costs to fix a failing dental implant placed abroad, variation in the standard of care, and lack of long- term aftercare and maintenance plan.
Should you wish to seek more information on dental implant therapy, please contact the practice on 01932857585 or get in touch online info@weybridgedentist.co.uk to arrange for a consultation. In that way, we can assess for your individual needs and provide you with a customised treatment plan .
Specialist treatment for gum disease affecting teeth and dental implants

Understanding the importance of gum health
Gum disease affects many aspects of our life but is often overlooked as it has few symptoms in its early stages – that’s why it is often called ‘the silent disease’.
The vital thing about gum disease is that it is highly preventable and, especially in the early stages, quite easily treatable. Many studies link oral health to a number of significant conditions. There is strong evidence of the links between diabetes and gum disease. For Alzheimer’s and cardio health the role of gum disease is less clear. More than 45% of adults in the UK are affected by gum disease and, even at its most mild level, it can affect your quality of life.
Gum disease can affect dental implants as much as natural teeth. If you have any concerns about your dentition, speak to us and we will be happy to work with your dentist in managing your case.
Saving Your Natural Tooth
Specialist Endodontic Treatment
Nothing looks, feels or functions like your natural teeth, and endodontists are the experts in saving teeth. Keep smiling and eating the foods you love with endodontic treatment that can relieve your pain and save your teeth.
Sometimes your teeth may have infection or disease and will need additional care. When possible, you should always consider treatments to save your teeth. You may think, why not have a tooth pulled, especially if no one can see it, but you will know your tooth is missing and it will negatively impact your quality of life.
Don’t get a tooth pulled because you think its easier or more cost-effective. Missing teeth can cause other teeth to shift, affect your ability to properly chew and ruin your smile. Tooth extraction often is more painful than the infection itself, and replacing an extracted tooth with an artificial one requires additional dental visits that can quickly add up.
Modern endodontics offers advancements in technologies, procedures and materials, giving you many treatment options to save your natural teeth. It’s important to understand your choices and how they’ll impact both your tooth and your future dental health. It’s always best to retain your natural teeth whenever possible and endodontic treatment should be your first choice for the best health and cosmetic results. Endodontists are specialists in saving teeth. They can evaluate your condition and provide the best treatment plan to help you save your teeth for a lifetime.
Here are some tips for saving your teeth:
- When given a choice between tooth extraction and root canal treatment, always opt for a root canal. No denture, bridge or implant will look, feel and function as well as a natural tooth.
- Act immediately when you experience symptoms of swelling or pain. Most endodontists can accommodate emergency cases, even on weekends, ensuring you’ll be seen quickly.
- If your dentist recommends tooth extraction, ask whether the root canal is an option.If you’re told root canal is not an option, ask why and request a referral to an endodontist.
Root canal treatment from an endodontist is virtually painless and often leaves you with less discomfort during recovery than if you have your natural tooth extracted. Thanks to modern techniques and effective anesthesia, patients who experience root canals are six times more likely to describe it as painless than patients who have a tooth extracted! Take the time to learn more about root canal treatment and some of the common misconceptions about it and then take the first step to a pain-free, healthy mouth by visiting an endodontist.
How does endodontic treatment save the tooth?
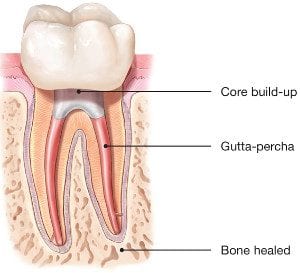
It’s necessary to have endodontic or root canal treatment when the inside of your tooth (the pulp) becomes inflamed or infected as a result of deep decay, repeated dental procedures, faulty crowns or a crack or chip in the tooth. Trauma to your tooth may also cause pulp damage even if the tooth has no visible chips or cracks. If pulp inflammation or infection is left untreated, it can cause pain or lead to an abscess.
When you undergo a root canal or other endodontic treatment, the inflamed or infected pulp is removed and the inside of the tooth is carefully cleaned and disinfected, then filled and sealed with a rubber-like material called gutta-percha. Afterward, the tooth is restored with a crown or filling for protection and will continue to function like any other tooth.
Endodontic treatment helps you maintain your natural smile, continue eating the foods you love and limits the need for ongoing dental work. With proper care, most teeth that have had root canal treatment can last a lifetime.
For more detailed information on root canal or to organise for a consultation, call us or get in touch online.
Biomimetic Dentistry
What is Biomimetic Dentistry?

Translated literally, biomimetic dentistry means to copy what is life-like. Nature has provided the most successful and ideal properties to our natural teeth. When restoring damaged, broken, and decayed teeth, the goal is to return the tooth to its original strength, function, and esthetics. Biomimetic dentistry accomplishes all of this in a conservative, strong, and attractive approach.
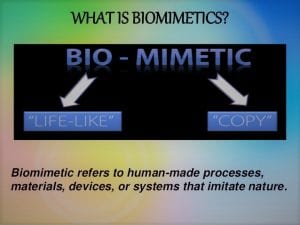
Why is it so important?
Tooth preservation and dental conservation lie at the heart of biomimetic dentistry.
Biomimetic dentistry replicates the strength, function, and aesthetics of natural teeth by replacing only damaged, decayed, and broken tooth structure. The principle employs techniques and materials that provide a perfect balance of nature, art and science.
Teeth move, bend and have physical dynamics of force that must be accounted for while re-making the tooth with nature as our guide. Much of the amputation of tooth structure can be eliminated with modern science. We can say that tooth preservation and dental conservation lie at the heart of biomimetic dentistry.
The economic implications of not needing the advanced, invasive care seen in traditional (amputational) dentistry have profound positive effects on people’s lives. We can now help patients create healthy and happy mouths with simple, and often painless techniques!
Patients are happier and often spend less compared to conventional treatment.
Give us a call to find out more or book a consultation appointment.
Want to stop snoring?
As a condition that affects over 40% of the population, it is no surprise that the majority of us have been impacted by snoring in some way, shape or form. There are both varying degrees and varying types of snoring: it can be ‘simple’, or it can be symptomatic and may require further exploration. Regardless, there are a number of conditions associated, including:
- diminished energy
- lack of concentration
- increased risk of stress
- reduced libido
- high blood pressure
As well as the impact to the snorer, a lack of sleep on the bed partner’s behalf is also dangerous for their health and well-being. Many cases are reported by the bed-partner, with the snorer having very little awareness of their bedtime activities.

Thankfully, there are many interventions that can assist with snoring. Before discussing these, however, it is first important to highlight the cause.
What causes snoring?
Once we are asleep, our muscles relax. This can result in the soft tissues in the throat vibrating, causing the familiar snoring sound.
However, this doesn’t happen to everyone: there are a number of factors that can increase chances of snoring, including: obesity, gender, age, alcohol, and medication. For most sufferers, snoring occurs in isolation (simple snoring). In these cases, it is often the bed-partner that suffers, with the snorer unaware that they are causing such a disturbance. However, it can also take place as part of a more serious condition, obstructive sleep apnoea, which can be potentially life-threatening if not treated correctly.
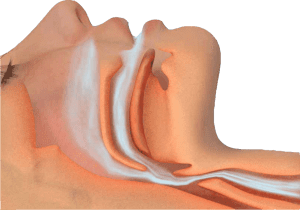
What is obstructive sleep apnoea (OSA)?
OSA is a serious condition where, for short periods of time, the airway becomes blocked during sleep, cutting off oxygen reaching the lungs. There are two types of breathing disruption associated with OSA:
- Apnoea – where the muscles collapse sufficiently enough to cause a total blockage of the airway for 10 seconds or more
- Hypopnoea – partial blockage of the airway that causes an airflow reduction of more than 50% for 10 seconds or more
Both of these problems can occur several times throughout the night and are most commonly recognised by loud snoring, paired with snorts, gasps, or laboured breathing. This leads to disruption for both the bed-partner AND the sufferer, with the snorer often waking feeling tired due to a night with reduced oxygen intake.
There are many associations with obstructive sleep apnoea, and, due to fat distribution, middle-aged males are twice as likely to suffer from OSA in comparison to middle-aged females. The discrepancy does start to level out, however, believed to be due to hormonal changes after menopause.
What are the treatments for snoring?
Though many snorers and tired bed-partners typically look to their doctor for help when it comes to snoring, their dentist arguably has a larger part to play – initially at least.
As snoring is typically caused by the lower jaw dropping back during sleep, the easiest way to stop it is to prevent the jaw from slipping backwards. This can be achieved with a device called a Mandibular Advancement Splint (MAS). Available from trained dentists, there are a number of devices available, one of which is the Sleepwell.

The most clinically proven MAS for the treatment of snoring & mild to moderate sleep apnoea, the Sleepwell is a two-piece device that is fully-adjustable by the wearer, and designed to hold your lower jaw forward. Holistically, however, there may be other behaviours that could assist with the problem, such as:
- Sleeping position – lying on your back inevitably is the worst position for snoring. Trying different positions may have a positive effect.
- Bed-time ‘hygiene’ – avoiding alcohol or caffeine in the evenings can help. Both muscle relaxants, they can increase the chances of snoring.
- Weight-loss – holding excess fat around your neck can play a major role in both snoring and sleep apnoea.
National Stop Snoring Week 23-27 April 2018
Cosmetic Dentistry- What You Should Know

Cosmetic dentistry has become increasingly popular, largely as a result of social trends and increased media coverage. This understandable desire for the alleged ‘perfect smile’ needs to be tempered with an appropriate awareness of the significant risks associated with invasive cosmetic procedures such as veneers and crowns. Patients need to be properly informed that elective removal of healthy enamel and dentine can result in pulpal injury and poorer periodontal health in the longer term, particularly if they are young. The duty of candour means that they ought to be informed that aggressive reduction of sound tooth tissue is not biologically neutral and results in structural weakening of their teeth. Less invasive procedures such as bleaching on its own or for example, combined with direct resin composite bonding, can satisfy many patient’s demands, while still being kinder to teeth and having much better fall-back positions for their future requirements. It is the opinion of the British Endodontic Society, British Society for Restorative Dentistry, Restorative Dentistry UK, Dental Trauma UK, British Society of Prosthodontics and the British Society of Paediatric Dentistry that elective invasive cosmetic dental treatments can result in great benefit to patients, but that some aggressive treatments used to achieve them can produce significant morbidities in teeth which were previously healthy. This is a worrying and growing problem with many ethical, legal and biologic aspects, but many adverse outcomes for patients who request cosmetic dental improvements are preventable by using biologically safer initial approaches to treatment planning and its provision.
Mouth Cancer Awareness Month

Most people have heard of cancer affecting parts of the body such as the lungs or breasts. However, cancer can also occur in the mouth, where the disease can affect the lips, tongue, cheeks and throat.
Anyone can be affected by mouth cancer, whether they have their own teeth or not. Mouth cancers are more common in people over 40, particularly men. However, research has shown that mouth cancer is becoming more common in younger patients and in women. In the last year more than 7,000 have been diagnosed with mouth cancer in the UK – an increase of more than a third compared to a decade ago.
Sadly, more than 1,800 people in the UK lose their life to mouth cancer every year. Many of these deaths could be prevented if the cancer was caught early enough. As it is, people with mouth cancer are more likely to die than those having cervical cancer or melanoma skin cancer.
Find out more at http://www.mouthcancer.org
Teeth whitening
Teeth whitening can be safe when done under the guidance of a dental professional or by following the instructions of over-the-counter products. However, it’s important to be aware of potential side effects, such as tooth sensitivity or gum irritation. Consult your dentist to discuss the best and safest whitening options for your specific needs.
Methods of teeth whitening:
**Professional Whitening:**This is done by a dentist and is the most effective method. It can involve in-office treatments using strong bleaching agents or custom-fitted trays with professional-grade whitening gels.
**Over-the-Counter (OTC) Products:** These include whitening toothpaste, strips, and gels. They are less potent than professional treatments and may take longer to show results.
Benefits of teeth whitening:
Improved Aesthetics: Whitening can remove stains and discoloration, enhancing the appearance of your teeth.
Boosted Confidence: A brighter smile often leads to increased self-confidence.
Non-Invasive: It’s a non-surgical and minimally invasive cosmetic dental procedure.
Risks and considerations:
Tooth Sensitivity: Whitening can cause temporary sensitivity to hot or cold foods and beverages.
Gum Irritation: Overuse or improper application of whitening products can irritate the gums.
Uneven Results: Whitening may not be equally effective on all teeth, leading to uneven results.
Duration of Effect: The duration of whitening effects varies; it may require touch-ups to maintain results.
Pre-existing Dental Issues: Whitening may not be suitable for everyone, especially those with dental restorations (crowns, fillings) as they do not respond to whitening treatments.
It’s crucial to consult with a dentist to discuss your specific needs and any potential risks associated with teeth whitening. They can help you choose the most appropriate and safe method for your situation.
Whitening Toothpastes; Facts and Fallacies
A Guide to Whitening Toothpastes in the UK: Efficacy Backed by Clinical Evidence
Whitening toothpastes are a popular choice for enhancing smiles, but how effective are they? In this blog, we’ll explore different types of whitening toothpastes available in the UK and evaluate their efficacy based on clinical evidence.
Abrasive-Based Whitening Toothpastes
These use mild abrasives like silica to remove surface stains caused by food, drinks, or smoking. While they can visibly improve brightness, clinical studies show they only remove extrinsic stains without altering the tooth’s natural color.
Efficacy: Effective for surface stain removal but not for deeper discoloration.
Enzyme-Based Whitening Toothpastes
Enzyme-based formulations (e.g., containing papain or bromelain) target protein pellicles that cause staining. Evidence suggests they can enhance stain removal without excessive abrasion, making them suitable for sensitive teeth.
Efficacy: Moderate improvement in surface brightness with minimal damage to enamel.
Peroxide-Based Whitening Toothpastes
Some toothpastes contain low levels of hydrogen or carbamide peroxide. Studies indicate they can help lighten intrinsic stains with consistent use over weeks. However, their whitening effect is less significant compared to professional bleaching.
Efficacy: Proven for mild intrinsic whitening, though results are subtle.
Charcoal Whitening Toothpastes
Charcoal-based products are widely marketed for whitening, but clinical evidence shows limited efficacy in removing stains. Excessive use may even harm enamel and gums due to high abrasiveness.
Efficacy: Poor stain removal with potential enamel damage.
Blue Covarine-Infused Toothpastes
These provide an immediate optical effect by depositing a blue pigment on teeth, creating the illusion of whiteness. While the results are temporary, studies support their effectiveness for a quick enhancement.
Efficacy: Temporary improvement in tooth brightness, ideal for short-term use.
Key Takeaways
Best for Surface Stains: Abrasive or enzyme-based toothpastes.
For Intrinsic Whitening: Peroxide-based formulas are most effective but offer mild results.
Quick Fix: Blue covarine toothpastes.
Avoid Overuse: Charcoal toothpastes due to abrasiveness.
For significant whitening or intrinsic stains, professional treatments remain the gold standard. Always consult your dentist to ensure the safest and most effective solution for your smile.
Dental Care and Coronavirus (COVID-19)
It is likely that the coronavirus will have an effect on your dental care.
Routine dental check-ups have been cancelled, and ongoing treatment plans may be disrupted. Where and how you access emergency dental treatment could also change.
This page includes advice on how you can access dental care, treatment and advice during the coronavirus pandemic.
Visiting the dental practice
If you are suffering with your oral health and need support, we are here to help.
To help stop the spread of coronavirus, we are advising against all routine and non-urgent dental treatment.
This includes:
Dental check-ups.
Preventive treatments such as scale and polish and fluoride varnishes.
Examinations and x-rays.
Appointments for braces.
Cosmetic dental treatment of any kind e.g. tooth whitening.
Routine denture treatment.
Treatments on teeth that are not painful e.g. fillings and extractions.
It is likely that your dental practice will contact you to postpone these appointments. If you do not hear from your dental practice, we recommend that you contact them to cancel your appointment and rearrange it for a later date.
In accordance to the instructions received by Public Health England (PHE) and CQC, all dental practices in England have temporarily ceased routine and non-urgent dental treatment. For emergency and urgent dental treatment, the dental surgery will provide remote (telephone or video-link) advice and assessment for further referral to the dedicated NHS Urgent Dental Care Centres (UDC) if necessary.
Whenever possible, stay at home and help stop the spread of coronavirus. This includes people of all ages – even if you do not have any symptoms or other health conditions.
Non-necessary dental treatment is not a reason for you to leave the home.
Urgent Dental Care
The NHS England has set up dedicated Urgent Dental Care Centres (UDC) for emergency and urgent dental conditions. Please note that this is not a walk-in service and requires appropriate referral by your dentist following remote triage.
If you are in pain, bleeding, swelling, or have had an accident and need urgent dental care, please contact your dental practice.
Please do not visit your dental practice without calling them first.
If you are not registered with any dental practice, please call 111 for further advice.
Dental Treatments in hospitals and A&E
To support NHS services and protect vital resources, it is important that you do not visit hospitals or A&E departments with dental problems.
If you need urgent or emergency dental treatment, contact your dental practice and they will be able to triage and direct you.
Dental care for vulnerable people and those with symptoms
If you need urgent dental care and are self-isolating because you have symptoms relating to coronavirus, or are a vulnerable person at higher risk, call NHS 111 or your dental practice.
The dental practice will be able to assess your needs and if necessary refer you to a special team/centre who will be able to treat you.
Buying oral health products
There is no shortage of oral health products like toothbrushes, toothpaste and mouthwash. Because of this, there is no need to stockpile them.
It is important to only buy what you need, when you need it.
Supermarkets remain open for essential food shopping and we advise that you buy any oral health products you need during this time. Please remember however to keep to social distancing rules and maintain two metres away from other shoppers.
When possible, instead of visiting supermarkets, we recommend that you buy oral health products online and have them delivered to your home.
Tips for good oral health
To help prevent dental problems from happening during coronavirus, here are some top tips for good oral health.
- Brush your teeth for two minutes, twice a day with a fluoride toothpaste.
- Do not share your toothbrushes. Keep the toothbrush clean and replace them frequently.
- The best time to brush is first thing in the morning and last thing at night before you go to bed.
- Cut down on how much sugar you have and how often you have it. This is even more important for children at home with increased temptation to snack and consume high sugar diet.
- Keep sugar consumption to mealtimes. This will reduce the time your teeth are under acid -attack.
- Maintain good hydration and avoid smoking and excessive consumption of alcohol.
- Use interdental brushes or floss to clean in between the teeth.
- Use non-alcohol based mouthwash daily to remove bad bacteria and keep fresh breath.
- Sugar-free chewing gum can help produce saliva and neutralise the plaque acids in your mouth.
More information and advice
Children coronavirus fact sheet, click here
For information about the coronavirus (COVID-19), please visit www.nhs.uk/conditions/coronavirus-covid-19/
The desire for the perfect Hollywood smile but at what cost?!

Cosmetic dentistry has become increasingly popular, largely as a result of social trends and increased media coverage. With the reality TV stars setting the trend in an industry now worth £2 billion, this understandable desire for the alleged ‘perfect smile’ needs to be tempered with an appropriate awareness of the significant risks associated with invasive cosmetic procedures such as veneers and crowns.
Patients need to be properly informed that elective removal of healthy enamel and dentine can result in pulpal injury and poorer periodontal health in the longer term, particularly if they are young. The duty of candour means that they ought to be informed that aggressive reduction of sound tooth tissue is not biologically neutral and results in structural weakening of their teeth. Less invasive procedures such as bleaching on its own or for example, combined with direct resin composite bonding, can satisfy many patient’s demands, while still being kinder to teeth and having much better fall-back positions for their future requirements.
It is the opinion of the British Endodontic Society, British Society for Restorative Dentistry, Restorative Dentistry UK, Dental Trauma UK, British Society of Prosthodontics and the British Society of Paediatric Dentistry that elective invasive cosmetic dental treatments can result in great benefit to patients, but that some aggressive treatments used to achieve them can produce significant morbidities in teeth which were previously healthy. This is a worrying and growing problem with many ethical, legal and biologic aspects, but many adverse outcomes for patients who request cosmetic dental improvements are preventable by using biologically safer initial approaches to treatment planning and its provision.
Dedicated personal, specialist care
The Specialist Dental Practice is the leading specialist restorative and implant dental practice in the county and has been setting the standards of specialist dentistry over the last 25 years.
The practice was established in 1973 and is conveniently located in the heart of Weybridge, Surrey. We are UK qualified and registered multi-specialist team offering specialist dental care of the highest quality and precision for the complex reconstruction cases involving dental implant therapy, gum disease treatment, root canal treatment, restoration of mutilated dentition and addressing challenges associated with partial and complete removable dentures.
We are delighted to welcome new referrals to our practice from both patients as well as professional colleagues.
Dental Implants
Essential questions to ask your dentist on dental implants
Taking the decision to have dental implants treatment is something most people will wish to consider quite carefully. Although this treatment can be an excellent long-term solution, it isn’t right for everybody and it is important to have a good understanding of exactly what is required. We have outlined a few essential questions and points you should be aware of before making your final decision.
WHAT ARE YOUR QUALIFICATIONS AND EXPERIENCE IN PLACING DENTAL IMPLANTS?
This is the most important question to ask and should be top of your list. Some clinicians have minimal training in placing dental implants and may only carry out this type of surgery a few times a year.
Our specialist care is based on dental specialties that are officially recognised by the General Dental Council UK. All accredited dental specialists are listed on the General Dental Council website www.gdc-uk.org. The specialist lists exist to:
• ensure high standards of training and assessment qualifying dentists to use a specialist title;
• indicate those dentists who possess recognised specialist knowledge, skills and attitudes;
• protect patients against unwarranted claims to be a specialist;
• facilitate appropriate referrals of patients;
• promote high standards of care by dentists qualified to use a specialist title; and
• encourage postgraduate education.
This list helps patients make an informed decision when they are looking for appropriately trained dentists to manage their dental care.
WHICH IMPLANT SYSTEMS DO YOU USE?
There are a few major dental implant companies that produce high-quality dental implants backed by years of research. These companies are well-known and well respected within the dental industry. There are numerous other companies that produce generic dental implants.
While these may still be of an acceptable quality, they lack the provenance of more widely known dental implant systems. There is another benefit of choosing dental implants made by one of the major companies as these implants are used worldwide. When you need an implant repaired or a component replaced or maintained, it is much easier to find a dentist willing to do this for you, no matter where you are in the world.
DO YOU PROVIDE COMPUTER GUIDED DENTAL IMPLANTS?
Computer guided dental implants surgery involves precisely planning using advanced diagnostics that include a cone beam CT scan and planning software. Once everything is planned, this computerised information is used to create a surgical guide or stent which allows precise placement of each implant.
We prefer to execute guided surgery where possible as it ensures your implant surgery is smoother, quicker and ultimately more comfortable and successful. Not all dentists will use this technique, but it is especially important when placing multiple implants where precision placement is even more vital.
Research shows that appropriately and precisely placed dental implants are less likely to have any problems and complications.
WILL IMPLANT SURGERY HURT?
You should not feel any pain during surgery based on effective local anaesthesia. We know many patients feel anxious at the thought of any oral surgery and if this applies to you then we can discuss additional sedation.
Our dental team is also very experienced at helping nervous patients feel at ease. Most of our patients will report no or very minimal discomfort that is very well managed with simple painkillers following implant surgery.
WILL I NEED A LONG TIME TO RECOVER AFTER IMPLANT SURGERY?
If you need just a single dental implant, you should be back to work the very next day. If you have multiple dental implants you might need a bit longer to recover; your dental implant dentist can give you more advice based on your situation.
Although you may feel some minor discomfort once the anaesthesia wears off, it is not uncommon to feel perfectly fine, especially after single dental implant placements. Again, this is something that can be discussed during your first consultation as it will depend on your treatment.
HOW LONG WILL IT TAKE TO COMPLETE IMPLANT TREATMENT?
Dental implant treatment can take up to several months to complete, as the surgery must be planned and once in place the implants need time to heal. It generally takes about 8-12 weeks for the dental implants to fully heal and to integrate with your jawbone, and the crown or bridge can be placed shortly after. Treatment may take slightly longer if you need bone grafts or tissue regeneration.
WILL I BE LEFT WITHOUT TEETH DURING IMPLANT HEALING?
This is a major concern for many people but there is no need to worry as temporary teeth can be provided while your implants heal. These temporary restorations can be fabricated before your implant surgery and may be placed immediately after surgery is completed.
WILL MY NEW IMPLANT TEETH LOOK NATURAL?
It is essential that your dental implants are placed in precisely the right position for the best functional and aesthetic effects. Here, at The Specialist dental Practice, our team are specialists in restoring and replacing missing teeth with crowns, bridges and dentures to the highest standards ensuring your new teeth are designed to look and feel wonderful. We also offer aftercare and advice on how to keep your implants clean.
HOW CAN I STOP MY DENTAL IMPLANTS FROM FAILING?
While some implants will fail naturally, a large part of implant success comes down to two factors:
• How well the implant is placed and the correct positioning in the jaw
• How well the implant is cared for after placement
Choosing a qualified and skilled implant dentist who is able to plan the correct positioning for your dental implants is key. Whilst you may think a general dentist is slightly cheaper, you may end up paying more in the future with implants that have not been placed correctly with significant potential complications.
The biggest misconception from dental implant patients is that once your dental implants are placed they will be there for life and are indestructible. The fact is, you will need to take care of your dental implants and make sure you regularly attend check-ups and clean your implants properly. Without this, your implants will have a larger chance of failing, both in a biologic and hardware sense.
SHOULD I GO ABROAD TO HAVE DENTAL IMPLANTS?
Dental tourism’ is a concept that has become increasingly popular over the last decade. Patients seek out dental treatment such as dental implants abroad and travel for the sole purpose of receiving cosmetic and restorative dentistry. The main attraction for patients is the cost of treatment in some other countries – it can look like prices are significantly cheaper, depending on the individual treatments. However, as with many things in life, what looks too good to be true often is. There are all kinds of hidden costs with choosing to get dental implants abroad including the prohibitive costs to fix a failing dental implant placed abroad, variation in the standard of care, and lack of long- term aftercare and maintenance plan.
Should you wish to seek more information on dental implant therapy, please contact the practice on 01932857585 or get in touch online info@weybridgedentist.co.uk to arrange for a consultation. In that way, we can assess for your individual needs and provide you with a customised treatment plan .
Specialist treatment for gum disease affecting teeth and dental implants

Understanding the importance of gum health
Gum disease affects many aspects of our life but is often overlooked as it has few symptoms in its early stages – that’s why it is often called ‘the silent disease’.
The vital thing about gum disease is that it is highly preventable and, especially in the early stages, quite easily treatable. Many studies link oral health to a number of significant conditions. There is strong evidence of the links between diabetes and gum disease. For Alzheimer’s and cardio health the role of gum disease is less clear. More than 45% of adults in the UK are affected by gum disease and, even at its most mild level, it can affect your quality of life.
Gum disease can affect dental implants as much as natural teeth. If you have any concerns about your dentition, speak to us and we will be happy to work with your dentist in managing your case.
Saving Your Natural Tooth
Specialist Endodontic Treatment
Nothing looks, feels or functions like your natural teeth, and endodontists are the experts in saving teeth. Keep smiling and eating the foods you love with endodontic treatment that can relieve your pain and save your teeth.
Sometimes your teeth may have infection or disease and will need additional care. When possible, you should always consider treatments to save your teeth. You may think, why not have a tooth pulled, especially if no one can see it, but you will know your tooth is missing and it will negatively impact your quality of life.
Don’t get a tooth pulled because you think its easier or more cost-effective. Missing teeth can cause other teeth to shift, affect your ability to properly chew and ruin your smile. Tooth extraction often is more painful than the infection itself, and replacing an extracted tooth with an artificial one requires additional dental visits that can quickly add up.
Modern endodontics offers advancements in technologies, procedures and materials, giving you many treatment options to save your natural teeth. It’s important to understand your choices and how they’ll impact both your tooth and your future dental health. It’s always best to retain your natural teeth whenever possible and endodontic treatment should be your first choice for the best health and cosmetic results. Endodontists are specialists in saving teeth. They can evaluate your condition and provide the best treatment plan to help you save your teeth for a lifetime.
Here are some tips for saving your teeth:
- When given a choice between tooth extraction and root canal treatment, always opt for a root canal. No denture, bridge or implant will look, feel and function as well as a natural tooth.
- Act immediately when you experience symptoms of swelling or pain. Most endodontists can accommodate emergency cases, even on weekends, ensuring you’ll be seen quickly.
- If your dentist recommends tooth extraction, ask whether the root canal is an option.If you’re told root canal is not an option, ask why and request a referral to an endodontist.
Root canal treatment from an endodontist is virtually painless and often leaves you with less discomfort during recovery than if you have your natural tooth extracted. Thanks to modern techniques and effective anesthesia, patients who experience root canals are six times more likely to describe it as painless than patients who have a tooth extracted! Take the time to learn more about root canal treatment and some of the common misconceptions about it and then take the first step to a pain-free, healthy mouth by visiting an endodontist.
How does endodontic treatment save the tooth?
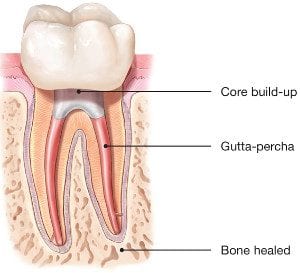
It’s necessary to have endodontic or root canal treatment when the inside of your tooth (the pulp) becomes inflamed or infected as a result of deep decay, repeated dental procedures, faulty crowns or a crack or chip in the tooth. Trauma to your tooth may also cause pulp damage even if the tooth has no visible chips or cracks. If pulp inflammation or infection is left untreated, it can cause pain or lead to an abscess.
When you undergo a root canal or other endodontic treatment, the inflamed or infected pulp is removed and the inside of the tooth is carefully cleaned and disinfected, then filled and sealed with a rubber-like material called gutta-percha. Afterward, the tooth is restored with a crown or filling for protection and will continue to function like any other tooth.
Endodontic treatment helps you maintain your natural smile, continue eating the foods you love and limits the need for ongoing dental work. With proper care, most teeth that have had root canal treatment can last a lifetime.
For more detailed information on root canal or to organise for a consultation, call us or get in touch online.
Biomimetic Dentistry
What is Biomimetic Dentistry?

Translated literally, biomimetic dentistry means to copy what is life-like. Nature has provided the most successful and ideal properties to our natural teeth. When restoring damaged, broken, and decayed teeth, the goal is to return the tooth to its original strength, function, and esthetics. Biomimetic dentistry accomplishes all of this in a conservative, strong, and attractive approach.
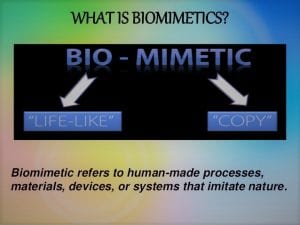
Why is it so important?
Tooth preservation and dental conservation lie at the heart of biomimetic dentistry.
Biomimetic dentistry replicates the strength, function, and aesthetics of natural teeth by replacing only damaged, decayed, and broken tooth structure. The principle employs techniques and materials that provide a perfect balance of nature, art and science.
Teeth move, bend and have physical dynamics of force that must be accounted for while re-making the tooth with nature as our guide. Much of the amputation of tooth structure can be eliminated with modern science. We can say that tooth preservation and dental conservation lie at the heart of biomimetic dentistry.
The economic implications of not needing the advanced, invasive care seen in traditional (amputational) dentistry have profound positive effects on people’s lives. We can now help patients create healthy and happy mouths with simple, and often painless techniques!
Patients are happier and often spend less compared to conventional treatment.
Give us a call to find out more or book a consultation appointment.
Want to stop snoring?
As a condition that affects over 40% of the population, it is no surprise that the majority of us have been impacted by snoring in some way, shape or form. There are both varying degrees and varying types of snoring: it can be ‘simple’, or it can be symptomatic and may require further exploration. Regardless, there are a number of conditions associated, including:
- diminished energy
- lack of concentration
- increased risk of stress
- reduced libido
- high blood pressure
As well as the impact to the snorer, a lack of sleep on the bed partner’s behalf is also dangerous for their health and well-being. Many cases are reported by the bed-partner, with the snorer having very little awareness of their bedtime activities.

Thankfully, there are many interventions that can assist with snoring. Before discussing these, however, it is first important to highlight the cause.
What causes snoring?
Once we are asleep, our muscles relax. This can result in the soft tissues in the throat vibrating, causing the familiar snoring sound.
However, this doesn’t happen to everyone: there are a number of factors that can increase chances of snoring, including: obesity, gender, age, alcohol, and medication. For most sufferers, snoring occurs in isolation (simple snoring). In these cases, it is often the bed-partner that suffers, with the snorer unaware that they are causing such a disturbance. However, it can also take place as part of a more serious condition, obstructive sleep apnoea, which can be potentially life-threatening if not treated correctly.
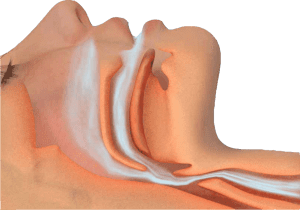
What is obstructive sleep apnoea (OSA)?
OSA is a serious condition where, for short periods of time, the airway becomes blocked during sleep, cutting off oxygen reaching the lungs. There are two types of breathing disruption associated with OSA:
- Apnoea – where the muscles collapse sufficiently enough to cause a total blockage of the airway for 10 seconds or more
- Hypopnoea – partial blockage of the airway that causes an airflow reduction of more than 50% for 10 seconds or more
Both of these problems can occur several times throughout the night and are most commonly recognised by loud snoring, paired with snorts, gasps, or laboured breathing. This leads to disruption for both the bed-partner AND the sufferer, with the snorer often waking feeling tired due to a night with reduced oxygen intake.
There are many associations with obstructive sleep apnoea, and, due to fat distribution, middle-aged males are twice as likely to suffer from OSA in comparison to middle-aged females. The discrepancy does start to level out, however, believed to be due to hormonal changes after menopause.
What are the treatments for snoring?
Though many snorers and tired bed-partners typically look to their doctor for help when it comes to snoring, their dentist arguably has a larger part to play – initially at least.
As snoring is typically caused by the lower jaw dropping back during sleep, the easiest way to stop it is to prevent the jaw from slipping backwards. This can be achieved with a device called a Mandibular Advancement Splint (MAS). Available from trained dentists, there are a number of devices available, one of which is the Sleepwell.

The most clinically proven MAS for the treatment of snoring & mild to moderate sleep apnoea, the Sleepwell is a two-piece device that is fully-adjustable by the wearer, and designed to hold your lower jaw forward. Holistically, however, there may be other behaviours that could assist with the problem, such as:
- Sleeping position – lying on your back inevitably is the worst position for snoring. Trying different positions may have a positive effect.
- Bed-time ‘hygiene’ – avoiding alcohol or caffeine in the evenings can help. Both muscle relaxants, they can increase the chances of snoring.
- Weight-loss – holding excess fat around your neck can play a major role in both snoring and sleep apnoea.
National Stop Snoring Week 23-27 April 2018
Cosmetic Dentistry- What You Should Know

Cosmetic dentistry has become increasingly popular, largely as a result of social trends and increased media coverage. This understandable desire for the alleged ‘perfect smile’ needs to be tempered with an appropriate awareness of the significant risks associated with invasive cosmetic procedures such as veneers and crowns. Patients need to be properly informed that elective removal of healthy enamel and dentine can result in pulpal injury and poorer periodontal health in the longer term, particularly if they are young. The duty of candour means that they ought to be informed that aggressive reduction of sound tooth tissue is not biologically neutral and results in structural weakening of their teeth. Less invasive procedures such as bleaching on its own or for example, combined with direct resin composite bonding, can satisfy many patient’s demands, while still being kinder to teeth and having much better fall-back positions for their future requirements. It is the opinion of the British Endodontic Society, British Society for Restorative Dentistry, Restorative Dentistry UK, Dental Trauma UK, British Society of Prosthodontics and the British Society of Paediatric Dentistry that elective invasive cosmetic dental treatments can result in great benefit to patients, but that some aggressive treatments used to achieve them can produce significant morbidities in teeth which were previously healthy. This is a worrying and growing problem with many ethical, legal and biologic aspects, but many adverse outcomes for patients who request cosmetic dental improvements are preventable by using biologically safer initial approaches to treatment planning and its provision.
Mouth Cancer Awareness Month

Most people have heard of cancer affecting parts of the body such as the lungs or breasts. However, cancer can also occur in the mouth, where the disease can affect the lips, tongue, cheeks and throat.
Anyone can be affected by mouth cancer, whether they have their own teeth or not. Mouth cancers are more common in people over 40, particularly men. However, research has shown that mouth cancer is becoming more common in younger patients and in women. In the last year more than 7,000 have been diagnosed with mouth cancer in the UK – an increase of more than a third compared to a decade ago.
Sadly, more than 1,800 people in the UK lose their life to mouth cancer every year. Many of these deaths could be prevented if the cancer was caught early enough. As it is, people with mouth cancer are more likely to die than those having cervical cancer or melanoma skin cancer.
Find out more at http://www.mouthcancer.org
Teeth whitening
Teeth whitening can be safe when done under the guidance of a dental professional or by following the instructions of over-the-counter products. However, it’s important to be aware of potential side effects, such as tooth sensitivity or gum irritation. Consult your dentist to discuss the best and safest whitening options for your specific needs.
Methods of teeth whitening:
**Professional Whitening:**This is done by a dentist and is the most effective method. It can involve in-office treatments using strong bleaching agents or custom-fitted trays with professional-grade whitening gels.
**Over-the-Counter (OTC) Products:** These include whitening toothpaste, strips, and gels. They are less potent than professional treatments and may take longer to show results.
Benefits of teeth whitening:
Improved Aesthetics: Whitening can remove stains and discoloration, enhancing the appearance of your teeth.
Boosted Confidence: A brighter smile often leads to increased self-confidence.
Non-Invasive: It’s a non-surgical and minimally invasive cosmetic dental procedure.
Risks and considerations:
Tooth Sensitivity: Whitening can cause temporary sensitivity to hot or cold foods and beverages.
Gum Irritation: Overuse or improper application of whitening products can irritate the gums.
Uneven Results: Whitening may not be equally effective on all teeth, leading to uneven results.
Duration of Effect: The duration of whitening effects varies; it may require touch-ups to maintain results.
Pre-existing Dental Issues: Whitening may not be suitable for everyone, especially those with dental restorations (crowns, fillings) as they do not respond to whitening treatments.
It’s crucial to consult with a dentist to discuss your specific needs and any potential risks associated with teeth whitening. They can help you choose the most appropriate and safe method for your situation.
Whitening Toothpastes; Facts and Fallacies
A Guide to Whitening Toothpastes in the UK: Efficacy Backed by Clinical Evidence
Whitening toothpastes are a popular choice for enhancing smiles, but how effective are they? In this blog, we’ll explore different types of whitening toothpastes available in the UK and evaluate their efficacy based on clinical evidence.
Abrasive-Based Whitening Toothpastes
These use mild abrasives like silica to remove surface stains caused by food, drinks, or smoking. While they can visibly improve brightness, clinical studies show they only remove extrinsic stains without altering the tooth’s natural color.
Efficacy: Effective for surface stain removal but not for deeper discoloration.
Enzyme-Based Whitening Toothpastes
Enzyme-based formulations (e.g., containing papain or bromelain) target protein pellicles that cause staining. Evidence suggests they can enhance stain removal without excessive abrasion, making them suitable for sensitive teeth.
Efficacy: Moderate improvement in surface brightness with minimal damage to enamel.
Peroxide-Based Whitening Toothpastes
Some toothpastes contain low levels of hydrogen or carbamide peroxide. Studies indicate they can help lighten intrinsic stains with consistent use over weeks. However, their whitening effect is less significant compared to professional bleaching.
Efficacy: Proven for mild intrinsic whitening, though results are subtle.
Charcoal Whitening Toothpastes
Charcoal-based products are widely marketed for whitening, but clinical evidence shows limited efficacy in removing stains. Excessive use may even harm enamel and gums due to high abrasiveness.
Efficacy: Poor stain removal with potential enamel damage.
Blue Covarine-Infused Toothpastes
These provide an immediate optical effect by depositing a blue pigment on teeth, creating the illusion of whiteness. While the results are temporary, studies support their effectiveness for a quick enhancement.
Efficacy: Temporary improvement in tooth brightness, ideal for short-term use.
Key Takeaways
Best for Surface Stains: Abrasive or enzyme-based toothpastes.
For Intrinsic Whitening: Peroxide-based formulas are most effective but offer mild results.
Quick Fix: Blue covarine toothpastes.
Avoid Overuse: Charcoal toothpastes due to abrasiveness.
For significant whitening or intrinsic stains, professional treatments remain the gold standard. Always consult your dentist to ensure the safest and most effective solution for your smile.
Dental Care and Coronavirus (COVID-19)
It is likely that the coronavirus will have an effect on your dental care.
Routine dental check-ups have been cancelled, and ongoing treatment plans may be disrupted. Where and how you access emergency dental treatment could also change.
This page includes advice on how you can access dental care, treatment and advice during the coronavirus pandemic.
Visiting the dental practice
If you are suffering with your oral health and need support, we are here to help.
To help stop the spread of coronavirus, we are advising against all routine and non-urgent dental treatment.
This includes:
Dental check-ups.
Preventive treatments such as scale and polish and fluoride varnishes.
Examinations and x-rays.
Appointments for braces.
Cosmetic dental treatment of any kind e.g. tooth whitening.
Routine denture treatment.
Treatments on teeth that are not painful e.g. fillings and extractions.
It is likely that your dental practice will contact you to postpone these appointments. If you do not hear from your dental practice, we recommend that you contact them to cancel your appointment and rearrange it for a later date.
In accordance to the instructions received by Public Health England (PHE) and CQC, all dental practices in England have temporarily ceased routine and non-urgent dental treatment. For emergency and urgent dental treatment, the dental surgery will provide remote (telephone or video-link) advice and assessment for further referral to the dedicated NHS Urgent Dental Care Centres (UDC) if necessary.
Whenever possible, stay at home and help stop the spread of coronavirus. This includes people of all ages – even if you do not have any symptoms or other health conditions.
Non-necessary dental treatment is not a reason for you to leave the home.
Urgent Dental Care
The NHS England has set up dedicated Urgent Dental Care Centres (UDC) for emergency and urgent dental conditions. Please note that this is not a walk-in service and requires appropriate referral by your dentist following remote triage.
If you are in pain, bleeding, swelling, or have had an accident and need urgent dental care, please contact your dental practice.
Please do not visit your dental practice without calling them first.
If you are not registered with any dental practice, please call 111 for further advice.
Dental Treatments in hospitals and A&E
To support NHS services and protect vital resources, it is important that you do not visit hospitals or A&E departments with dental problems.
If you need urgent or emergency dental treatment, contact your dental practice and they will be able to triage and direct you.
Dental care for vulnerable people and those with symptoms
If you need urgent dental care and are self-isolating because you have symptoms relating to coronavirus, or are a vulnerable person at higher risk, call NHS 111 or your dental practice.
The dental practice will be able to assess your needs and if necessary refer you to a special team/centre who will be able to treat you.
Buying oral health products
There is no shortage of oral health products like toothbrushes, toothpaste and mouthwash. Because of this, there is no need to stockpile them.
It is important to only buy what you need, when you need it.
Supermarkets remain open for essential food shopping and we advise that you buy any oral health products you need during this time. Please remember however to keep to social distancing rules and maintain two metres away from other shoppers.
When possible, instead of visiting supermarkets, we recommend that you buy oral health products online and have them delivered to your home.
Tips for good oral health
To help prevent dental problems from happening during coronavirus, here are some top tips for good oral health.
- Brush your teeth for two minutes, twice a day with a fluoride toothpaste.
- Do not share your toothbrushes. Keep the toothbrush clean and replace them frequently.
- The best time to brush is first thing in the morning and last thing at night before you go to bed.
- Cut down on how much sugar you have and how often you have it. This is even more important for children at home with increased temptation to snack and consume high sugar diet.
- Keep sugar consumption to mealtimes. This will reduce the time your teeth are under acid -attack.
- Maintain good hydration and avoid smoking and excessive consumption of alcohol.
- Use interdental brushes or floss to clean in between the teeth.
- Use non-alcohol based mouthwash daily to remove bad bacteria and keep fresh breath.
- Sugar-free chewing gum can help produce saliva and neutralise the plaque acids in your mouth.
More information and advice
Children coronavirus fact sheet, click here
For information about the coronavirus (COVID-19), please visit www.nhs.uk/conditions/coronavirus-covid-19/
The desire for the perfect Hollywood smile but at what cost?!

Cosmetic dentistry has become increasingly popular, largely as a result of social trends and increased media coverage. With the reality TV stars setting the trend in an industry now worth £2 billion, this understandable desire for the alleged ‘perfect smile’ needs to be tempered with an appropriate awareness of the significant risks associated with invasive cosmetic procedures such as veneers and crowns.
Patients need to be properly informed that elective removal of healthy enamel and dentine can result in pulpal injury and poorer periodontal health in the longer term, particularly if they are young. The duty of candour means that they ought to be informed that aggressive reduction of sound tooth tissue is not biologically neutral and results in structural weakening of their teeth. Less invasive procedures such as bleaching on its own or for example, combined with direct resin composite bonding, can satisfy many patient’s demands, while still being kinder to teeth and having much better fall-back positions for their future requirements.
It is the opinion of the British Endodontic Society, British Society for Restorative Dentistry, Restorative Dentistry UK, Dental Trauma UK, British Society of Prosthodontics and the British Society of Paediatric Dentistry that elective invasive cosmetic dental treatments can result in great benefit to patients, but that some aggressive treatments used to achieve them can produce significant morbidities in teeth which were previously healthy. This is a worrying and growing problem with many ethical, legal and biologic aspects, but many adverse outcomes for patients who request cosmetic dental improvements are preventable by using biologically safer initial approaches to treatment planning and its provision.
Dedicated personal, specialist care
The Specialist Dental Practice is the leading specialist restorative and implant dental practice in the county and has been setting the standards of specialist dentistry over the last 25 years.
The practice was established in 1973 and is conveniently located in the heart of Weybridge, Surrey. We are UK qualified and registered multi-specialist team offering specialist dental care of the highest quality and precision for the complex reconstruction cases involving dental implant therapy, gum disease treatment, root canal treatment, restoration of mutilated dentition and addressing challenges associated with partial and complete removable dentures.
We are delighted to welcome new referrals to our practice from both patients as well as professional colleagues.
Dental Implants
Essential questions to ask your dentist on dental implants
Taking the decision to have dental implants treatment is something most people will wish to consider quite carefully. Although this treatment can be an excellent long-term solution, it isn’t right for everybody and it is important to have a good understanding of exactly what is required. We have outlined a few essential questions and points you should be aware of before making your final decision.
WHAT ARE YOUR QUALIFICATIONS AND EXPERIENCE IN PLACING DENTAL IMPLANTS?
This is the most important question to ask and should be top of your list. Some clinicians have minimal training in placing dental implants and may only carry out this type of surgery a few times a year.
Our specialist care is based on dental specialties that are officially recognised by the General Dental Council UK. All accredited dental specialists are listed on the General Dental Council website www.gdc-uk.org. The specialist lists exist to:
• ensure high standards of training and assessment qualifying dentists to use a specialist title;
• indicate those dentists who possess recognised specialist knowledge, skills and attitudes;
• protect patients against unwarranted claims to be a specialist;
• facilitate appropriate referrals of patients;
• promote high standards of care by dentists qualified to use a specialist title; and
• encourage postgraduate education.
This list helps patients make an informed decision when they are looking for appropriately trained dentists to manage their dental care.
WHICH IMPLANT SYSTEMS DO YOU USE?
There are a few major dental implant companies that produce high-quality dental implants backed by years of research. These companies are well-known and well respected within the dental industry. There are numerous other companies that produce generic dental implants.
While these may still be of an acceptable quality, they lack the provenance of more widely known dental implant systems. There is another benefit of choosing dental implants made by one of the major companies as these implants are used worldwide. When you need an implant repaired or a component replaced or maintained, it is much easier to find a dentist willing to do this for you, no matter where you are in the world.
DO YOU PROVIDE COMPUTER GUIDED DENTAL IMPLANTS?
Computer guided dental implants surgery involves precisely planning using advanced diagnostics that include a cone beam CT scan and planning software. Once everything is planned, this computerised information is used to create a surgical guide or stent which allows precise placement of each implant.
We prefer to execute guided surgery where possible as it ensures your implant surgery is smoother, quicker and ultimately more comfortable and successful. Not all dentists will use this technique, but it is especially important when placing multiple implants where precision placement is even more vital.
Research shows that appropriately and precisely placed dental implants are less likely to have any problems and complications.
WILL IMPLANT SURGERY HURT?
You should not feel any pain during surgery based on effective local anaesthesia. We know many patients feel anxious at the thought of any oral surgery and if this applies to you then we can discuss additional sedation.
Our dental team is also very experienced at helping nervous patients feel at ease. Most of our patients will report no or very minimal discomfort that is very well managed with simple painkillers following implant surgery.
WILL I NEED A LONG TIME TO RECOVER AFTER IMPLANT SURGERY?
If you need just a single dental implant, you should be back to work the very next day. If you have multiple dental implants you might need a bit longer to recover; your dental implant dentist can give you more advice based on your situation.
Although you may feel some minor discomfort once the anaesthesia wears off, it is not uncommon to feel perfectly fine, especially after single dental implant placements. Again, this is something that can be discussed during your first consultation as it will depend on your treatment.
HOW LONG WILL IT TAKE TO COMPLETE IMPLANT TREATMENT?
Dental implant treatment can take up to several months to complete, as the surgery must be planned and once in place the implants need time to heal. It generally takes about 8-12 weeks for the dental implants to fully heal and to integrate with your jawbone, and the crown or bridge can be placed shortly after. Treatment may take slightly longer if you need bone grafts or tissue regeneration.
WILL I BE LEFT WITHOUT TEETH DURING IMPLANT HEALING?
This is a major concern for many people but there is no need to worry as temporary teeth can be provided while your implants heal. These temporary restorations can be fabricated before your implant surgery and may be placed immediately after surgery is completed.
WILL MY NEW IMPLANT TEETH LOOK NATURAL?
It is essential that your dental implants are placed in precisely the right position for the best functional and aesthetic effects. Here, at The Specialist dental Practice, our team are specialists in restoring and replacing missing teeth with crowns, bridges and dentures to the highest standards ensuring your new teeth are designed to look and feel wonderful. We also offer aftercare and advice on how to keep your implants clean.
HOW CAN I STOP MY DENTAL IMPLANTS FROM FAILING?
While some implants will fail naturally, a large part of implant success comes down to two factors:
• How well the implant is placed and the correct positioning in the jaw
• How well the implant is cared for after placement
Choosing a qualified and skilled implant dentist who is able to plan the correct positioning for your dental implants is key. Whilst you may think a general dentist is slightly cheaper, you may end up paying more in the future with implants that have not been placed correctly with significant potential complications.
The biggest misconception from dental implant patients is that once your dental implants are placed they will be there for life and are indestructible. The fact is, you will need to take care of your dental implants and make sure you regularly attend check-ups and clean your implants properly. Without this, your implants will have a larger chance of failing, both in a biologic and hardware sense.
SHOULD I GO ABROAD TO HAVE DENTAL IMPLANTS?
Dental tourism’ is a concept that has become increasingly popular over the last decade. Patients seek out dental treatment such as dental implants abroad and travel for the sole purpose of receiving cosmetic and restorative dentistry. The main attraction for patients is the cost of treatment in some other countries – it can look like prices are significantly cheaper, depending on the individual treatments. However, as with many things in life, what looks too good to be true often is. There are all kinds of hidden costs with choosing to get dental implants abroad including the prohibitive costs to fix a failing dental implant placed abroad, variation in the standard of care, and lack of long- term aftercare and maintenance plan.
Should you wish to seek more information on dental implant therapy, please contact the practice on 01932857585 or get in touch online info@weybridgedentist.co.uk to arrange for a consultation. In that way, we can assess for your individual needs and provide you with a customised treatment plan .
Specialist treatment for gum disease affecting teeth and dental implants

Understanding the importance of gum health
Gum disease affects many aspects of our life but is often overlooked as it has few symptoms in its early stages – that’s why it is often called ‘the silent disease’.
The vital thing about gum disease is that it is highly preventable and, especially in the early stages, quite easily treatable. Many studies link oral health to a number of significant conditions. There is strong evidence of the links between diabetes and gum disease. For Alzheimer’s and cardio health the role of gum disease is less clear. More than 45% of adults in the UK are affected by gum disease and, even at its most mild level, it can affect your quality of life.
Gum disease can affect dental implants as much as natural teeth. If you have any concerns about your dentition, speak to us and we will be happy to work with your dentist in managing your case.
Saving Your Natural Tooth
Specialist Endodontic Treatment
Nothing looks, feels or functions like your natural teeth, and endodontists are the experts in saving teeth. Keep smiling and eating the foods you love with endodontic treatment that can relieve your pain and save your teeth.
Sometimes your teeth may have infection or disease and will need additional care. When possible, you should always consider treatments to save your teeth. You may think, why not have a tooth pulled, especially if no one can see it, but you will know your tooth is missing and it will negatively impact your quality of life.
Don’t get a tooth pulled because you think its easier or more cost-effective. Missing teeth can cause other teeth to shift, affect your ability to properly chew and ruin your smile. Tooth extraction often is more painful than the infection itself, and replacing an extracted tooth with an artificial one requires additional dental visits that can quickly add up.
Modern endodontics offers advancements in technologies, procedures and materials, giving you many treatment options to save your natural teeth. It’s important to understand your choices and how they’ll impact both your tooth and your future dental health. It’s always best to retain your natural teeth whenever possible and endodontic treatment should be your first choice for the best health and cosmetic results. Endodontists are specialists in saving teeth. They can evaluate your condition and provide the best treatment plan to help you save your teeth for a lifetime.
Here are some tips for saving your teeth:
- When given a choice between tooth extraction and root canal treatment, always opt for a root canal. No denture, bridge or implant will look, feel and function as well as a natural tooth.
- Act immediately when you experience symptoms of swelling or pain. Most endodontists can accommodate emergency cases, even on weekends, ensuring you’ll be seen quickly.
- If your dentist recommends tooth extraction, ask whether the root canal is an option.If you’re told root canal is not an option, ask why and request a referral to an endodontist.
Root canal treatment from an endodontist is virtually painless and often leaves you with less discomfort during recovery than if you have your natural tooth extracted. Thanks to modern techniques and effective anesthesia, patients who experience root canals are six times more likely to describe it as painless than patients who have a tooth extracted! Take the time to learn more about root canal treatment and some of the common misconceptions about it and then take the first step to a pain-free, healthy mouth by visiting an endodontist.
How does endodontic treatment save the tooth?
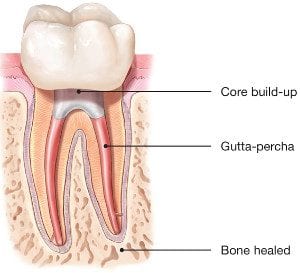
It’s necessary to have endodontic or root canal treatment when the inside of your tooth (the pulp) becomes inflamed or infected as a result of deep decay, repeated dental procedures, faulty crowns or a crack or chip in the tooth. Trauma to your tooth may also cause pulp damage even if the tooth has no visible chips or cracks. If pulp inflammation or infection is left untreated, it can cause pain or lead to an abscess.
When you undergo a root canal or other endodontic treatment, the inflamed or infected pulp is removed and the inside of the tooth is carefully cleaned and disinfected, then filled and sealed with a rubber-like material called gutta-percha. Afterward, the tooth is restored with a crown or filling for protection and will continue to function like any other tooth.
Endodontic treatment helps you maintain your natural smile, continue eating the foods you love and limits the need for ongoing dental work. With proper care, most teeth that have had root canal treatment can last a lifetime.
For more detailed information on root canal or to organise for a consultation, call us or get in touch online.
Biomimetic Dentistry
What is Biomimetic Dentistry?

Translated literally, biomimetic dentistry means to copy what is life-like. Nature has provided the most successful and ideal properties to our natural teeth. When restoring damaged, broken, and decayed teeth, the goal is to return the tooth to its original strength, function, and esthetics. Biomimetic dentistry accomplishes all of this in a conservative, strong, and attractive approach.
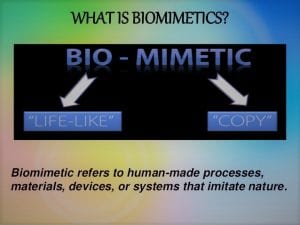
Why is it so important?
Tooth preservation and dental conservation lie at the heart of biomimetic dentistry.
Biomimetic dentistry replicates the strength, function, and aesthetics of natural teeth by replacing only damaged, decayed, and broken tooth structure. The principle employs techniques and materials that provide a perfect balance of nature, art and science.
Teeth move, bend and have physical dynamics of force that must be accounted for while re-making the tooth with nature as our guide. Much of the amputation of tooth structure can be eliminated with modern science. We can say that tooth preservation and dental conservation lie at the heart of biomimetic dentistry.
The economic implications of not needing the advanced, invasive care seen in traditional (amputational) dentistry have profound positive effects on people’s lives. We can now help patients create healthy and happy mouths with simple, and often painless techniques!
Patients are happier and often spend less compared to conventional treatment.
Give us a call to find out more or book a consultation appointment.
Want to stop snoring?
As a condition that affects over 40% of the population, it is no surprise that the majority of us have been impacted by snoring in some way, shape or form. There are both varying degrees and varying types of snoring: it can be ‘simple’, or it can be symptomatic and may require further exploration. Regardless, there are a number of conditions associated, including:
- diminished energy
- lack of concentration
- increased risk of stress
- reduced libido
- high blood pressure
As well as the impact to the snorer, a lack of sleep on the bed partner’s behalf is also dangerous for their health and well-being. Many cases are reported by the bed-partner, with the snorer having very little awareness of their bedtime activities.

Thankfully, there are many interventions that can assist with snoring. Before discussing these, however, it is first important to highlight the cause.
What causes snoring?
Once we are asleep, our muscles relax. This can result in the soft tissues in the throat vibrating, causing the familiar snoring sound.
However, this doesn’t happen to everyone: there are a number of factors that can increase chances of snoring, including: obesity, gender, age, alcohol, and medication. For most sufferers, snoring occurs in isolation (simple snoring). In these cases, it is often the bed-partner that suffers, with the snorer unaware that they are causing such a disturbance. However, it can also take place as part of a more serious condition, obstructive sleep apnoea, which can be potentially life-threatening if not treated correctly.
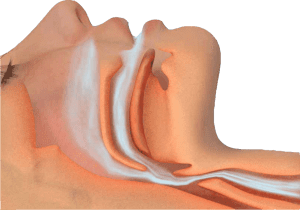
What is obstructive sleep apnoea (OSA)?
OSA is a serious condition where, for short periods of time, the airway becomes blocked during sleep, cutting off oxygen reaching the lungs. There are two types of breathing disruption associated with OSA:
- Apnoea – where the muscles collapse sufficiently enough to cause a total blockage of the airway for 10 seconds or more
- Hypopnoea – partial blockage of the airway that causes an airflow reduction of more than 50% for 10 seconds or more
Both of these problems can occur several times throughout the night and are most commonly recognised by loud snoring, paired with snorts, gasps, or laboured breathing. This leads to disruption for both the bed-partner AND the sufferer, with the snorer often waking feeling tired due to a night with reduced oxygen intake.
There are many associations with obstructive sleep apnoea, and, due to fat distribution, middle-aged males are twice as likely to suffer from OSA in comparison to middle-aged females. The discrepancy does start to level out, however, believed to be due to hormonal changes after menopause.
What are the treatments for snoring?
Though many snorers and tired bed-partners typically look to their doctor for help when it comes to snoring, their dentist arguably has a larger part to play – initially at least.
As snoring is typically caused by the lower jaw dropping back during sleep, the easiest way to stop it is to prevent the jaw from slipping backwards. This can be achieved with a device called a Mandibular Advancement Splint (MAS). Available from trained dentists, there are a number of devices available, one of which is the Sleepwell.

The most clinically proven MAS for the treatment of snoring & mild to moderate sleep apnoea, the Sleepwell is a two-piece device that is fully-adjustable by the wearer, and designed to hold your lower jaw forward. Holistically, however, there may be other behaviours that could assist with the problem, such as:
- Sleeping position – lying on your back inevitably is the worst position for snoring. Trying different positions may have a positive effect.
- Bed-time ‘hygiene’ – avoiding alcohol or caffeine in the evenings can help. Both muscle relaxants, they can increase the chances of snoring.
- Weight-loss – holding excess fat around your neck can play a major role in both snoring and sleep apnoea.
National Stop Snoring Week 23-27 April 2018
Cosmetic Dentistry- What You Should Know

Cosmetic dentistry has become increasingly popular, largely as a result of social trends and increased media coverage. This understandable desire for the alleged ‘perfect smile’ needs to be tempered with an appropriate awareness of the significant risks associated with invasive cosmetic procedures such as veneers and crowns. Patients need to be properly informed that elective removal of healthy enamel and dentine can result in pulpal injury and poorer periodontal health in the longer term, particularly if they are young. The duty of candour means that they ought to be informed that aggressive reduction of sound tooth tissue is not biologically neutral and results in structural weakening of their teeth. Less invasive procedures such as bleaching on its own or for example, combined with direct resin composite bonding, can satisfy many patient’s demands, while still being kinder to teeth and having much better fall-back positions for their future requirements. It is the opinion of the British Endodontic Society, British Society for Restorative Dentistry, Restorative Dentistry UK, Dental Trauma UK, British Society of Prosthodontics and the British Society of Paediatric Dentistry that elective invasive cosmetic dental treatments can result in great benefit to patients, but that some aggressive treatments used to achieve them can produce significant morbidities in teeth which were previously healthy. This is a worrying and growing problem with many ethical, legal and biologic aspects, but many adverse outcomes for patients who request cosmetic dental improvements are preventable by using biologically safer initial approaches to treatment planning and its provision.
Mouth Cancer Awareness Month

Most people have heard of cancer affecting parts of the body such as the lungs or breasts. However, cancer can also occur in the mouth, where the disease can affect the lips, tongue, cheeks and throat.
Anyone can be affected by mouth cancer, whether they have their own teeth or not. Mouth cancers are more common in people over 40, particularly men. However, research has shown that mouth cancer is becoming more common in younger patients and in women. In the last year more than 7,000 have been diagnosed with mouth cancer in the UK – an increase of more than a third compared to a decade ago.
Sadly, more than 1,800 people in the UK lose their life to mouth cancer every year. Many of these deaths could be prevented if the cancer was caught early enough. As it is, people with mouth cancer are more likely to die than those having cervical cancer or melanoma skin cancer.
Find out more at http://www.mouthcancer.org
FIND US

Address
25 Monument Green
Weybridge
Surrey
KT13 8QW

Telephone
01932857585
Hours
Monday—Thursday: 9:00AM–5:30PM
Friday: 9:00AM–1:00PM
The surgery is closed at weekends and Public Holidays
The Specialist Dental Practice
Weybridge dentist providing dedicated personal, specialist care.
Akil Gulamali Limited. Registered Office: 2 Minton Place, Victoria Road, Bicester, England, OX26 6QB. Registered in England and Wales 9284784.
© 2024 The Specialist Dental Practice. All rights reserved.